The article by Dr. Gustavo R. Zubieta-Calleja and colleagues in published as open access in Reviews on Recent Clinical Trials, 2020
Credit: Dr. Gustavo R. Zubieta-Calleja and colleagues, Bentham Science Publishers
The current COVID-19 pandemic has caused over 1 million deaths which can be attributed to its severe progressive pulmonary compromise. The necessity to understand this disease has resulted in detailed analyses of its transmission and clinical aspects published worldwide. In this recent report, doctors in Bolivia provide, who live and work at more than 3,600m from above sea level, a high altitude specialists’ perspective. At high-altitude, hypoxemia (low oxygen in the blood), the main complication in COVID-19, is every day’s life experience at the High Altitude Pulmonary and Pathology Institute (HAPPI-IPPA) in La Paz, Bolivia, for 50+ years. Unlike high altitude illnesses, according to Prof. Dr. Gustavo Zubieta-Calleja, COVID-19 presents his transcendental new concept: “pneumolysis” (pneumo=lung, lysis=destruction).
View the video on the research: https:/
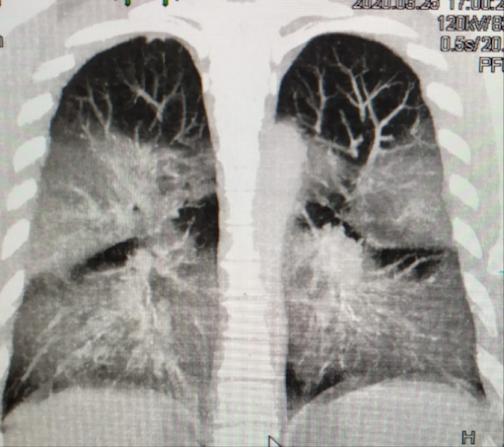
Initially, all physicians worldwide assumed that the lung affliction in COVID-19 (evidenced by CAT scans and caused by SARS-CoV-2) was the same as in older strains SARS-CoV. However, as fatality rates increased in Intensive Care Units, it became evident that this pathology was entirely new.
The SARS-CoV-2 virus enters the body through inhalation of the viral load, and travels through the bronchi to the surface of the alveoli respiratory sacs where pneumocytes (alveolar lung cells), and their capillaries are located. The pneumocytes allow the diffusion of oxygen molecules to the capillaries where red blood cells capture and transport them to all tissues. They also allow the passage of carbon dioxide molecules (a waste product of respiration) to be exhaled.
SARS-CoV-2 penetrates pneumocytes through the ACE2 receptors and starts self-replication of its RNA within. Pneumocytes are eventually destroyed liberating all replicated SARS-CoV-2 RNA that further infect other adjacent pneumocytes. The paper authored by Prof. Dr. Gustavo Zubieta-Calleja, suggests that multiple diseases may arise from SARS-CoV-2 entering the capillaries.
The coronavirus intrusion gradually reduces the lung’s gas exchange area. This results in alveoli inflammation and a superimposed alteration of lung function similar to High Altitude Pulmonary Edema (HAPE). Both in COVID-19 and HAPE, sea level patients cannot take in enough oxygen as if they were rapidly placed on the summit of Mt. Everest, without time for adaptation. Nevertheless, HAPE is entirely reversible as its mechanism is different, and there is no destruction of alveoli.
The extreme hypoxemia experienced in COVID-19 patients leads physicians to use ventilators (a mechanical way of pumping air into the lungs) to improve oxygenation. However, using high pressures on partially destroyed and fragile lungs can result in the worst outcomes. Whereas non-invasive ventilation results in better outcomes.
If patients survive the acute pneumolysis with critically low oxygen levels in COVID-19, recovery results in irreversible fibrosis (scars) in the lungs. This damaged tissue is no longer useful for gas exchange, so compensation can be commonly achieved by increasing the number of red blood cells (hemoglobin oxygen transporters). This poly-erythrocythemia) is a compensation mechanism found in high-altitude residents who suffer chronic lung diseases or other oxygen transport disorders, commonly known as “Chronic Mountain Sickness”.
In COVID-19, sea level hemoglobin can also become insufficient. The authors postulate that a fundamental treatment strategy to increase the transport of oxygen could be erythropoietin. This hormone naturally increases red blood cell production and protects the heart, brain, and vessels from hypoxia’s hazards.
Prompt administration of oxygen is important as it can reduce the formation of HAPE-type edema and cardiopulmonary overwork. The use of anti-inflammatory medication, being tops Aspirin for its analgesic, anti-inflammatory, anti-fever, and anti-coagulation effects, are also proposed. Timely use of antibiotics (to protect from super-infection), adequate oral rehydration, antitussives (promoting a resting lung) and other anti-coagulation drugs should also be considered on each individual case.
To allow people to return to work, Dr. Zubieta-Calleja proposes the use of space type earth suits with electric ventilator open circuit adequately filtered air, reducing contagion risk. The CoV-2 is a natural biological cleansing mechanism attacking more severely those with decreased immunity, inflammatory processes, or overlapping diseases. “The individual ultimate survival tool under COVID-19 presence…” as he explains: “is a strong immune system”.
###
The team’s observations were originally published on May 5th, 2020 as a pre-print at
https:/
CONTACT:
Prof. Dr. Gustavo Zubieta-Calleja
Head
High Altitude Pulmonary & Pathology Institute (HAPPI – IPPA)
Cell: +591 73258026
AltitudeClinic.com
[email protected]
The article is published in the journal, Reviews on Recent Clinical Trials. To read the full-text article please visit: https:/
Media Contact
Faizan ul Haq
[email protected]
Related Journal Article
http://dx.




