Credit: WFIRM
WINSTON-SALEM, NC, NOVEMBER, 2020 — Wake Forest Institute for Regenerative Medicine scientists (WFIRM) have developed a method to bioprint a type of cartilage that could someday help restore knee function damaged by arthritis or injury.
This cartilage, known as fibrocartilage, helps connect tendons or ligaments or bones and is primarily found in the meniscus in the knee. The meniscus is the tough, rubbery cartilage that acts as a shock absorber in the knee joint. Degeneration of the meniscus tissue affects millions of patients and arthroscopic partial meniscectomy is one of the most common orthopedic operations performed. Besides surgery, there is a lack of available treatment options.
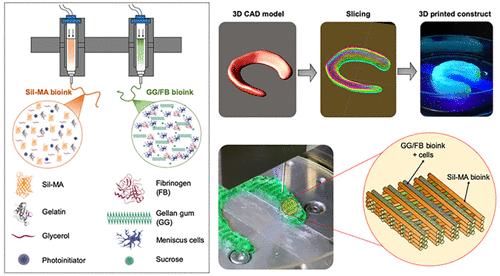
In this latest proof-of-concept strategy, the scientists have been able to 3D bioprint a hybrid tissue construct for cartilage regeneration by printing two specialized bioinks – hydrogels that contain the cells – together to create a new formulation that provides a cell-friendly microenvironment and structural integrity. This work is done with the Integrated Tissue and Organ Printing System, a 3D bioprinter that was developed by WFIRM researchers over a 14-year period. The system deposits both biodegradable, plastic-like materials to form the tissue “shape” and bioinks that contain the cells to build new tissues and organs.
“In this study, we have been able to produce a highly elastic hybrid construct for advanced fibrocartilaginous regeneration,” said Sang Jin Lee, Ph.D, associate professor at WFIRM and author of the paper recently published by Chemistry of Materials journal. “The results demonstrate that this bioprinted construct offers a versatile and promising alternative for the production of this type of tissue.”
For the study, Lee and the WFIRM research team tested various formulations and measured response to applied forces or stresses, the swelling ratio and the material strength and flexibility. One provided the proper cellular microenvironment to maintain the cells and helping them grow while the other bioink offered excellent biomechanical behavior and structural integrity. The final formula of the two bioinks used were co-printed layer by layer to create a mesh-like pattern. The constructs were implanted into a small animal model for observation for 10 weeks and evaluated at intermittent time periods, showing proper function.
“A larger preclinical study will be needed to further examine the body’s response and the functional recovery of the joint with use of this regenerative medicine treatment,” said James Yoo, MD, PhD, professor at WFIRM.
“We have such a need for effective treatments and therapies to help patients deal with degenerative joint problems, especially the knee,” said Anthony Atala, MD, director of WFIRM. “This proof-of-concept study helps point our work in the right direction to someday be able to engineer this crucial tissue that is so important for patients.”
###
Co-authors include: Jihoon Park and Adam M. Jorgensen of WFIRM; Joao B. Costa, Joana Silva-Correia, Rui L. Reis, and Joaquim M. Oliveira.
This study was supported by National Institutes of Health grant (1P41EB023833-346 01) and the Portuguese Foundation for Science and Technology (PTDC/BBB-ECT/2690/2014 and PTDC/EMD-EMD/31367/2017).
Authors Atala, Lee and Yoo are inventors on patent rights related to the Integrated Tissue and Organ Printing System work owned by Wake Forest University Health Sciences. The patents, whose value may be affected by publication, have the potential to generate royalty income in which the inventors would share.
About the Wake Forest Institute for Regenerative Medicine: The Wake Forest Institute for Regenerative Medicine is recognized as an international leader in translating scientific discovery into clinical therapies, with many world firsts, including the development and implantation of the first engineered organ in a patient. Over 400 people at the institute, the largest in the world, work on more than 40 different tissues and organs. A number of the basic principles of tissue engineering and regenerative medicine were first developed at the institute. WFIRM researchers have successfully engineered replacement tissues and organs in all four categories – flat structures, tubular tissues, hollow organs and solid organs – and 15 different applications of cell/tissue therapy technologies, such as skin, urethras, cartilage, bladders, muscle, kidney, and vaginal organs, have been successfully used in human patients. The institute, which is part of Wake Forest School of Medicine, is located in the Innovation Quarter in downtown Winston-Salem, NC, and is driven by the urgent needs of patients. The institute is making a global difference in regenerative medicine through collaborations with over 400 entities and institutions worldwide, through its government, academic and industry partnerships, its start-up entities, and through major initiatives in breakthrough technologies, such as tissue engineering, cell therapies, diagnostics, drug discovery, biomanufacturing, nanotechnology, gene editing and 3D printing.
Media Contact
Bonnie Davis
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




