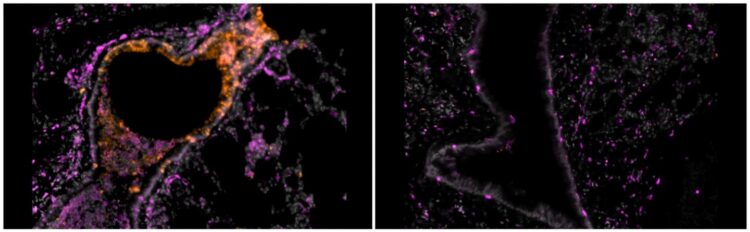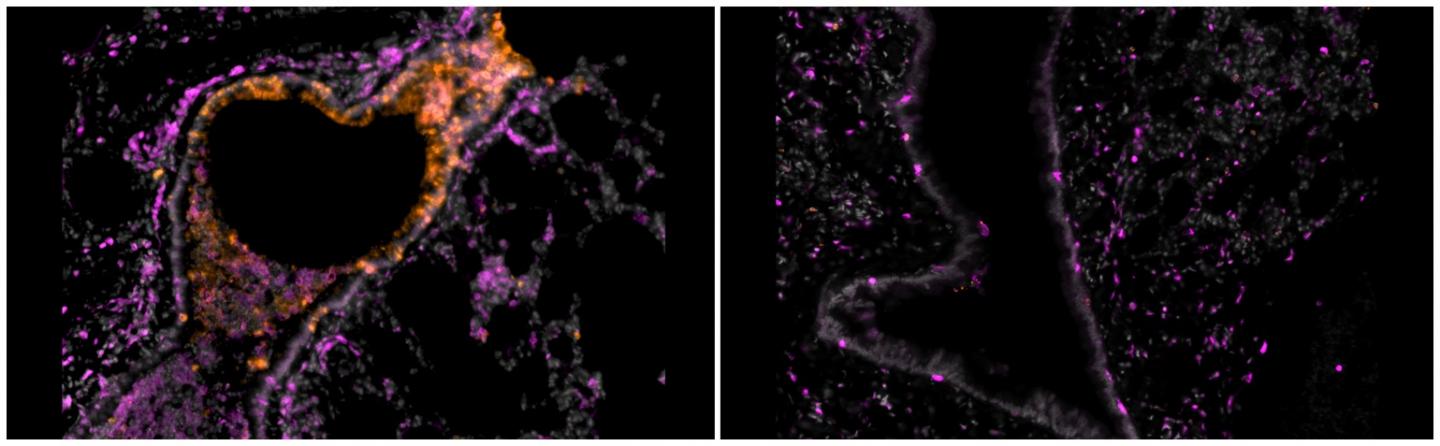
Credit: Nambulli et al., Science Advances
PITTSBURGH, May 26, 2021 – In a paper published today in Science Advances, researchers from the University of Pittsburgh School of Medicine showed that inhalable nanobodies targeting the spike protein of the SARS-CoV-2 coronavirus can prevent and treat severe COVID-19 in hamsters. This is the first time the nanobodies–which are similar to monoclonal antibodies but smaller in size, more stable and cheaper to produce–were tested for inhalation treatment against coronavirus infections in a pre-clinical model.
The scientists showed that low doses of an aerosolized nanobody named Pittsburgh inhalable Nanobody-21 (PiN-21) protected hamsters from the dramatic weight loss typically associated with severe SARS-CoV-2 infection and reduced the number of infectious virus particles in the animals’ nasal cavities, throats and lungs by a million-fold, compared to placebo treatment with a nanobody that doesn’t neutralize the virus.
“By using an inhalation therapy that can be directly administered to the infection site–the respiratory tract and lungs–we can make treatments more efficient,” said co-senior author Yi Shi, Ph.D., assistant professor of cell biology at Pitt. “We are very excited and encouraged by our data suggesting that PiN-21 can be highly protective against severe disease and can potentially prevent human-to-human viral transmission.”
Previously, Shi and colleagues discovered a large repertoire of over 8,000 high-affinity SARS-CoV-2 nanobodies. From this repertoire, the scientists selected an ultrapotent nanobody (Nb21) and bioengineered it into a trimeric form to further maximize its antiviral activity. The resulting PiN-21 is by far the most potent antiviral nanobody that has been identified, according to the researchers’ review of published studies.
The experiments showed that PiN-21 was protective when administered intranasally at the time of infection. Hamsters in the PiN-21 treatment group did not lose any body weight, unlike the placebo-treated animals who lost up to 16% of their initial body weight after a week of infection. For the average adult human, the rate of the weight loss would correspond to shedding roughly 20 pounds in a week.
Even more impressively, inhalation of aerosolized nanobodies at an ultra-low dose reduced the number of infectious virus particles in the lung tissue by 6-logs (or a million-fold). Animals who received aerosolized PiN-21 nanobodies had milder changes in the lung structure and a lower degree of inflammation than those who received the placebo.
To deliver therapeutics via aerosolization, the scientists had to overcome several technical challenges–small particle aerosols have to reach deep into the lung, and treatment particles need to be small enough so that they don’t clump together and strong enough to withstand the extreme pressure required to suspend them in the air. PiN-21 nanobodies, which are approximately four times smaller than typical monoclonal antibodies with exceptionally high stability, are perfectly suited for the task. They also are much cheaper to produce and can be generated rapidly to swiftly adapt to the shape-shifting virus.
“COVID-19 is now a preeminent disease of the 21st century,” said co-author Doug Reed, Ph.D., associate professor of immunology at Pitt. “Delivering the treatment directly to the lungs can make a big difference for our ability to treat it.”
Researchers point out that the nanobodies and vaccines are complementary and do not compete with one another. Vaccines remain the best tool to stop the virus from spreading from person to person, but nanobodies will be useful to treat people who already are sick and those who can’t get vaccinated for other medical reasons.
Promising early preclinical data, combined with the researchers’ extensive knowledge about rapidly identifying drug-quality nanobodies, suggest that this approach can provide a convenient and cost-effective therapeutic option to control the coronavirus pandemic.
“This work is the result of experts in nanobody production, infectious disease and aerobiology working closely together. At the University of Pittsburgh Center for Vaccine Research, we don’t just talk about ideas, we actually make them come to life,” said co-senior author Paul Duprex, Ph.D., the center’s director.
###
Other authors on the manuscript include Sham Nambulli, Ph.D., Natasha Tilston-Lunel, Ph.D., Linda J. Rennick, Ph.D., William Klimstra, Ph.D., all of the Pitt Center for Vaccine Research; Yufei Xiang, M.S., of Pitt’s Department of Cell Biology; Zhe Sang, M.S., of Pittsburgh-Carnegie Mellon University Program in Computational Biology; and Nicholas Crossland, Ph.D., of Boston University.
This work was supported by the National Institutes of Health (grant #1R35GM137905-01), a University of Pittsburgh Clinical and Translational Science Institute pilot grant, the University of Pittsburgh, the Pitt Center for Vaccine Research, the Commonwealth of Pennsylvania Department of Community and Economic Development, the Richard King Mellon Foundation and the Henry L. Hillman Foundation.
Shi and Xiang are inventors on a pending patent related to this work filed by University of Pittsburgh (no. 63067567, filed on Aug. 28, 2020).
To read this release online or share it, visit https:/
About the University of Pittsburgh School of Medicine
As one of the nation’s leading academic centers for biomedical research, the University of Pittsburgh School of Medicine integrates advanced technology with basic science across a broad range of disciplines in a continuous quest to harness the power of new knowledge and improve the human condition. Driven mainly by the School of Medicine and its affiliates, Pitt has ranked among the top 10 recipients of funding from the National Institutes of Health since 1998. In rankings recently released by the National Science Foundation, Pitt ranked fifth among all American universities in total federal science and engineering research and development support.
Likewise, the School of Medicine is equally committed to advancing the quality and strength of its medical and graduate education programs, for which it is recognized as an innovative leader, and to training highly skilled, compassionate clinicians and creative scientists well-equipped to engage in world-class research. The School of Medicine is the academic partner of UPMC, which has collaborated with the University to raise the standard of medical excellence in Pittsburgh and to position health care as a driving force behind the region’s economy. For more information about the School of Medicine, see http://www.
http://www.
Media Contact
Anastasia Gorelova
[email protected]