Irvine, CA – June 23, 2021 – A new University of California, Irvine-led study finds that the persistence of a marker of chronic cellular stress, previously associated with neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD), also takes place in the brains of Huntington’s disease (HD) patients.
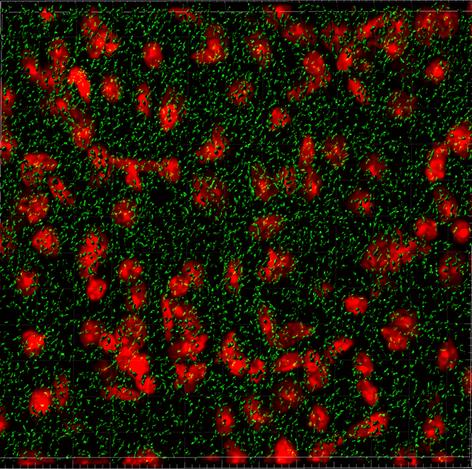
Chronic cellular stress results in the abnormal accumulation of stress granules (SGs), which are clumps of protein and RNAs that gather in the cell. Prior to this study, published in the Journal of Clinical Investigation, it was not known if these types of granules were a pathological feature of HD, an inherited and progressive neurodegenerative disorder that typically strikes in the prime of life.
In addition to identifying SGs as a pathological feature of HD, researchers made several other discoveries including that extracellular vesicles, which float in cerebrospinal fluid (CSF) and act as a messaging system between cells in the brain, can potentially alter the behavior of other cells and impact the abnormal accumulation of the granules. They also found that TAR DNA-binding protein 43 (TDP43) is mislocalized, which has emerged as a critical feature of multiple neurodegenerative diseases.
“We were initially interested in whether the profile of these messages could serve as a biomarker for HD and investigated whether the vesicles from HD patients contain messages that are different from those of unaffected individuals,” said first author Isabella I. Sanchez, PhD, from the Thompson Laboratory at UCI School of Medicine.
Researchers found that the CSF of HD patients carried messages in the form of small non-coding RNAs (miRNAs) that did were predicted to alter the production of proteins that are indispensable for SG formation. They soon identified a key player in SG dynamics, GTPase-activating protein-binding protein 1 (G3BP1), as a predicted target.
“This finding regarding the miRNAs was very exciting, as we had simultaneously started investigations to characterize SGs in HD brain tissues. SGs can be very difficult to detect in brain tissues, and it just so happened that we had narrowed down the adequate conditions and were ready to being characterizing G3BP1 SGs in HD mouse and HD patient brains,” said Leslie M. Thompson, PhD, Donald Bren and UCI Chancellor’s professor in the Departments of Psychiatry & Human Behavior and Biological Chemistry at the UCI School of Medicine, and Neurobiology and Behavior at the UCI School of Biological Sciences.
While SG formation is a normal physiological process that enables cells to overcome stressful conditions, the SG pathology in HD may result from an accumulation G3BP1 SGs that initially served a protective function, but develop into hyper-stable structures over time.
###
This research was supported in part by grants from the Medical Research Council, CHDI Foundation, the National Institutes of Health, Chan Zuckerberg Initiative, National Center for Research Resources, National Center for Advancing Translational Sciences, and the UCI Institute for Clinical & Translational Science.
About the UCI School of Medicine
Each year, the UCI School of Medicine educates more than 400 medical students, and nearly 150 doctoral and master’s students. More than 700 residents and fellows are trained at UCI Medical Center and affiliated institutions. The School of Medicine offers an MD; a dual MD/PhD medical scientist training program; and PhDs and master’s degrees in anatomy and neurobiology, biomedical sciences, genetic counseling, epidemiology, environmental health sciences, pathology, pharmacology, physiology and biophysics, and translational sciences. Medical students also may pursue an MD/MBA, an MD/master’s in public health, or an MD/master’s degree through one of three mission-based programs: Health Education to Advance Leaders in Integrative Medicine (HEAL-IM), Leadership Education to Advance Diversity-African, Black and Caribbean (LEAD-ABC), and the Program in Medical Education for the Latino Community (PRIME-LC). The UCI School of Medicine is accredited by the Liaison Committee on Medical Accreditation and ranks among the top 50 nationwide for research. For more information, visit som.uci.edu.
Media Contact
Anne Warde
[email protected]
Original Source
https:/
Related Journal Article
http://dx.