Scaffold-aided repair led to stronger meniscus, laying groundwork for potential human tests
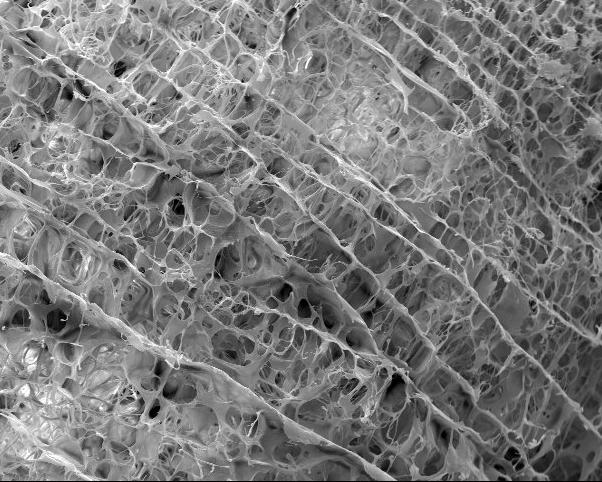
Credit: Duke Health
DURHAM, N.C. – About a million times a year, Americans with a torn meniscus in their knee undergo surgery in hopes of a repair. Certain tears can’t be fixed or won’t heal well, and many patients later suffer osteoarthritis from the injury.
Scientists have tried developing scaffolds or structures from various materials, including plastic and textile fibers, to lay a foundation for new cells. In a paper published June 18 in the journal Scientific Reports, Duke scientists describe a more organic model — a scaffold derived from a pig’s meniscus, which performed better in lab tests than healing without a scaffold.
“A partial meniscus removal is one of the most commonly performed orthopedic surgeries in the U.S.,” said Amy McNulty, Ph.D., an assistant professor in orthopedic surgery at Duke and senior author of the paper.
“The damaged tissue must be cut out because it’s causing pain or catching, but when the tissue comes out it also alters load-bearing in the knee and often leads to osteoarthritis, so it would be beneficial to try and heal the meniscus in place using a tool like a scaffold,” McNulty said.
In lab tests, repairs aided by the scaffold resulted in a stronger meniscus repair after four weeks compared to a meniscus that went through the natural healing process.
A scaffold could be especially valuable when the meniscus tears near the inside of the crescent-shaped tissue where blood doesn’t flow. Without a blood supply, a tear in this section won’t mend and the tissue is often removed, McNulty said.
The pig-derived scaffold is advantageous over other models including synthetics, because it is processed without chemicals or enzymes, which helps it retain more natural properties, McNulty said. Also, the structure is more porous than other models and even regular meniscus tissue, which allows new cells to move into it more easily to integrate with damaged tissue.
“Cells from the native tissue appear to be naturally attracted to the scaffold — they want to move into it,” McNulty said. “Hopefully, this will lead one day to a scaffold being placed into different tears to augment healing and seamlessly integrate the pieces of damaged tissue.”
The next step is testing the scaffold in animal models and eventually in humans, she said.
###
In addition to McNulty, study authors include Jacob C. Ruprecht, Taylor D. Waanders, Christopher R. Rowland, James F. Nishimuta, Katherine A. Glass, Jennifer Stencel, Louis E. DeFrate, Farshid Guilak and J. Brice Weinberg.
The research was supported by the National Institutes of Health (grants AG028716, AR048852, AG015768, AR073752, AG046927, AR073221, AR074800, and AR065527), the Arthritis Foundation, a U.S. Department of Veterans Affairs Rehabilitation Research Service Merit Review Award, the Lord Foundation in support of the Shared Materials Instrumentation Facility Undergraduate User Program and an Orthopaedic Research and Education Foundation grant with funding provided by the Musculoskeletal Transplant Foundation.
Media Contact
Samiha Khanna
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




