A team of researchers from Massachusetts General Hospital (MGH) and the Rowland Institute at Harvard University have used a specialized nanoprobe developed by the Harvard/Rowland investigators to directly measure levels of key proteins within living, cultured cells. As described in the journal Nano Letters, the investigators used the device to track levels of the Alzheimer’s-disease-associated proteins amyloid-beta (A-beta) and tau in neurons and other cells exposed to an anesthetic known to produce Alzheimer’s-like changes in the brains of mice. Their results support the view that the generation of A-beta is among the first steps leading to the characteristic neurodegeneration of Alzheimer’s disease.
“To study the dynamics of A-beta and tau, we needed a way to trigger the expression of both proteins and a tool to track dynamic changes of protein expression,” says lead author Feng Liang, PhD, a research fellow at the Rowland Institute.
In 2008, some of the MGH members of the current team showed that the anesthetic isoflurane induced characteristic changes seen in Alzheimer’s disease – including activation of cell-death enzymes and generation of A-beta – in cultured cells and in mouse brains. In 2014, the Harvard/Rowland researchers demonstrated the ability of their nanodevice to detect levels of intracellular proteins in living, cultured cells. The current study merges both of these accomplishments to investigate a key question regarding the mechanism of Alzheimer’s disease – whether generation of A-beta precedes or follows the generation of the abnormal form of tau that characterizes the disease.
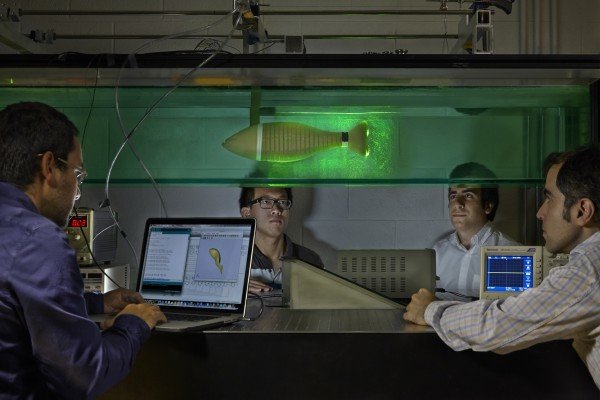
The tip of the device developed by the Harvard/Rowland investigators is around 50 nanometers (billionths of a meter) across, about 200 times smaller than a single cell. An integrated gold nanorod serves as the biosensor for what is called surface plasmon resonance – an oscillation of electrons in response to a light signal that can generate an optical readout reflecting protein binding signals. Antibodies targeting specific proteins can be integrated into the probe to give specific measurements of protein levels. The team first demonstrated that it was possible to use the nanoplasmonic fiber tip probe (nFTP) to quantify protein levels in individual cells without affecting their vitality and viability.
Using the nFTP device the investigators then tracked the changing levels of A-beta and the Alzheimer’s-associated form of tau, which is characterized by excess phosphate molecules, in cultured cells that had been treated with isoflurane. The readings indicated that the increase in A-beta expression preceded the rise in phosphorylated tau levels by several hours. The team then showed that, while blocking A-beta expression reduced tau levels, blocking tau did not prevent the initial rise in A-beta. However, without phosphorylated tau expression, A-beta levels eventually began to drop, suggesting a sequence in which A-beta generation stimulates tau phosphorylation, which promotes further generation of A-beta.
“We have brought the traditional immunoassay into living cells with exquisite sensitivity,” says Qimin Quan, PhD, a junior fellow at the Rowland Institute and co-corresponding author of the Nano Letters report. “The device is still limited in its ability to measure a large number of single cells, requiring further improvement. But its high-sensitivity, label-free and single-cell capability make it a unique tool for diagnosing clinically obtained limited samples.”
Zhongcong Xie, MD, PhD, director of the Geriatric Anesthesia Research Unit in the MGH Department of Anesthesia, Critical Care and Pain Medicine and co-corresponding author of the study, adds, “Each year approximately 8.5 million patients with Alzheimer’s disease need anesthesia and surgical care worldwide. Learning how anesthesia affects the mechanisms behind Alzheimer’s will require collaboration among specialists in anesthesia, neurology and engineering. Moreover, this use of both an anesthetic and the nFTP device to measure interactions between A-beta and tau is just a first step.” Xie is a professor of Anesthesia at Harvard Medical School.
###
Additional co-authors of the Nano Letters study are Yiying Zhang, MD and Yuanlin Dong, MD, MGH Anesthesia; Wooyoung Hong, PhD, Harvard Department of Chemistry and Chemical Biology. Support for the study includes a Rowland Junior Fellowship award and National Institutes of Health grants R01 GM088801, R01 AG041274 and HD 086977.
The Rowland Institute was originally founded by the late Edwin H. Land in 1980 as The Rowland Institute for Science, a privately endowed, nonprofit, basic research organization, conceived to advance science in a wide variety of fields. The Rowland Junior Fellows Program lies at the heart of the Institute: A program dedicated to experimental science over a broad range of disciplines for young investigators. Current research is carried out in physics, chemistry, biophysics, and biology, with an emphasis on interdisciplinary work and the development of new experimental tools. The Institute is located in Cambridge, Massachusetts near the Longfellow Bridge.
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH Research Institute conducts the largest hospital-based research program in the nation, with an annual research budget of more than $800 million and major research centers in HIV/AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, photomedicine and transplantation biology.
Media Contact
Terri Ogan
[email protected]
617-726-0954
@MassGeneralNews
http://www.mgh.harvard.edu
The post Nanoprobe enables measurement of protein dynamics in living cells appeared first on Scienmag.