A device that can monitor the levels of specific drugs as they flow through the bloodstream may soon take the guesswork out of drug dosing and allow physicians to tailor prescriptions to their patients’ specific biology.
Developed by UC Santa Barbara researchers Tom Soh, Kevin Plaxco and Scott Ferguson, the biosensor combines engineering and biochemistry and has far-reaching potential.
Doctors and pharmaceutical companies can generally determine reasonable drug doses for most patients through batteries of tests and trials. However, the efficacy of a drug treatment relies on maintaining therapeutic levels of the drug in the body, a feat not so easily accomplished.
“Current dosing regimens are really quite primitive,” said Plaxco, professor of chemistry and of biomolecular science and engineering. They rely on a patient’s age or body weight and are unable to account for specific responses over time. Drug levels may be influenced by individual patients’ metabolisms, or even by the foods they eat or other drugs they might be taking. When coupled with the primitive state of current dosing algorithms, this variability can be quite dangerous for drugs that have narrow therapeutic ranges. That in turn both doctor and patient to balance on the fine line between effectiveness and toxicity.
Scientists could be one giant step closer to dispelling the uncertainty around patients’ biological responses as they receive these drugs with a device that is only a bit longer than a jumbo paperclip. Called MEDIC (Microfluidic Electrochemical Detector for In vivo Continuous monitoring), the instrument can determine — continuously and in real time — concentrations of specific molecules in tiny amounts of whole blood. The kind of information it can provide could lead to truly personalized medicine.
“The easier and faster your doctor can detect specific molecules — drug molecules, proteins that are diagnostic of a specific disease — the faster your doctor can diagnose disease and monitor treatment,” said Plaxco.
This work is the result of a multiyear collaboration among the research labs of professors Plaxco; Soh, Ruth Garland Chair and professor of mechanical engineering, chemical engineering and materials; and Tod Kippin from the Department of Psychological and Brain Sciences. The MEDIC device consists of a microfluidic chamber lined with gold electrodes from which drug- recognizing biomolecules — in this case artificial DNA strands called aptamers — extend. When the target molecule comes in contact with an aptamer, the strand recognizes it and wraps around the molecule, delivering electrons from its tip to the electrode at the aptamer’s base. The tiny jolt of current signals the presence of the molecule.
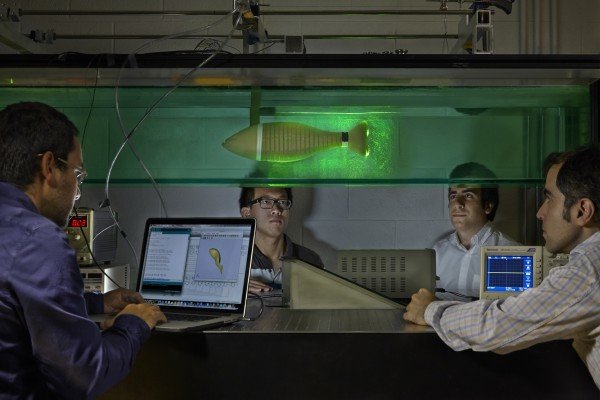
“For the first time, we can see how the body is processing specific molecules,” said Ferguson, a postdoctoral researcher in the Soh lab and the lead author of the study. Ferguson invented the central technology for continuously monitoring drug levels in whole blood, an element of time that is necessary to provide a full picture of how an individual responds to a certain drug. Previous iterations of the device would fail after about half an hour, because the components in whole blood — proteins and coagulants — are sticky and would cling to the sensors, gumming up the works.
For Ferguson it became a mechanical engineering problem, one he solved by introducing a second flow into the chamber, a liquid buffer on the sensors that stacked right on top of the bloodstream without mixing with or disturbing it. The buffer was the ideal environment for the aptamers and acted like a filter, separating the large blood components from the small drug molecules.
“We took a classic approach, which is to exploit differences in diffusivity: Big stuff diffuses slowly, while small stuff diffuses much more quickly,” Ferguson said.
“Think of swimmers,” he explained, “swimming from one bank of a river to another across a fast-moving current. The faster swimmers can make it across the stream, while the slower swimmers get carried downstream by the current.” In this way, the slower, larger blood components continue to move along the blood flow stream while the smaller, faster-moving molecules can cross from the blood flow through the buffer to the sensors.”
“The device worked incredibly well,” said Kippin, whose lab tested the microfluidic device. “The measurements were highly sensitive to doses that are clinically relevant and could be maintained for several hours. Further, we demonstrated exquisite selectivity and flexibility in that the device is only sensitive to the target even when administered a cocktail of drugs.”
MEDIC is still in the early clinical stages, and approvals for medical use may be some years away, but its effectiveness is opening up doors of opportunity and progress that Soh can already see. In the short term, the device can make available the kind of data necessary for critical advances in drug therapy.
“It can measure one’s metabolism in real time so you can deliver the drug in the right amount,” said Soh.
This capability may also have potential effects in the world of pharmaceuticals, in which newly developed drugs have to undergo rigourous testing and often fall short.
“A lot of drugs fail in phase three clinical trials, and it’s very expensive for the drug companies. Phase three is the hurdle in which it has to work in a broad general population,” Soh explained. With advanced real-time continuous monitoring, drugs that may have been effective for some but not for others may be adjusted to improve their performance and ultimately provide a wider choice of therapies.
Additionally, aptamers are relatively easy biosensors to produce and can be evolved to target the proteins that are indicators of disease, aiding in more sophisticated diagnostics. Several layers of different sensors may even be put in the same device to monitor several targets at the same time.
The next step for the researchers is to be able to deliver drugs automatically, with dosages based on the feedback generated by the device. An artificial pancreas, which monitors glucose levels in diabetics and uses this information to inject a controlled dose of insulin, is an example of one such system. UCSB researchers in chemical engineering recently helped develop an artificial pancreas system, which has been in clinical trials in conjunction with insulin therapies for type 1 diabetes.
“The ability to do feedback is really critical for a lot of diseases,” said Soh. Chemotherapy, for instance, where the therapeutic range is narrow for many drugs and patients need continuous infusions, could benefit from a continuous feedback loop between patient and pump.
“In the long term, we could use this feedback to control broken biological systems,” he said.
Story Source:
The above story is based on materials provided by The University of California – Santa Barbara.