The Next-Generation Copy Number Alteration (NG-CNA) assay can analyze small amounts of material to estimate metastatic risk, reports The Journal of Molecular Diagnostics
Credit: The Journal of Molecular Diagnostics
Philadelphia, December 12, 2018 – For men newly diagnosed with prostate cancer or patients previously treated, the risk of metastasis is a crucial determinant of whether to choose conservative management or undergo further treatment. For prostate as well as other cancers, primary tumor growth or spread is driven by amplifications or deletions of portions of the genome known as copy number alterations (CNAs). A report in The Journal of Molecular Diagnostics describes a new assay to assess CNAs that is cheaper, faster, reproducible, and requires less tissue than other diagnostic techniques and has the potential to significantly enhance prostate cancer evaluation.
Metastases occur in approximately 16 percent of prostate cancers and account for 8 percent of all male cancer deaths. Accurate prediction at the time of diagnosis can identify men at risk for metastasis who would benefit from aggressive therapy. Detection of CNAs in prostate tissue or blood can provide an indication whether previously diagnosed disease has progressed. The amplified and deleted genes represent novel targets for treating aggressive prostate cancer.
“We have demonstrated that CNAs can be detected rapidly and accurately with the new Next-Generation Copy Number Alteration (NG-CNA) assay. The impact of this information is two-fold: to assure aggressive therapy at the time of diagnosis for men with metastasis-prone disease and provide a rationale for active surveillance (and not overtreatment) for men with indolent disease,” explained lead investigator Harry Ostrer, MD, of the Department of Pathology, Albert Einstein College of Medicine, Bronx, NY, USA.
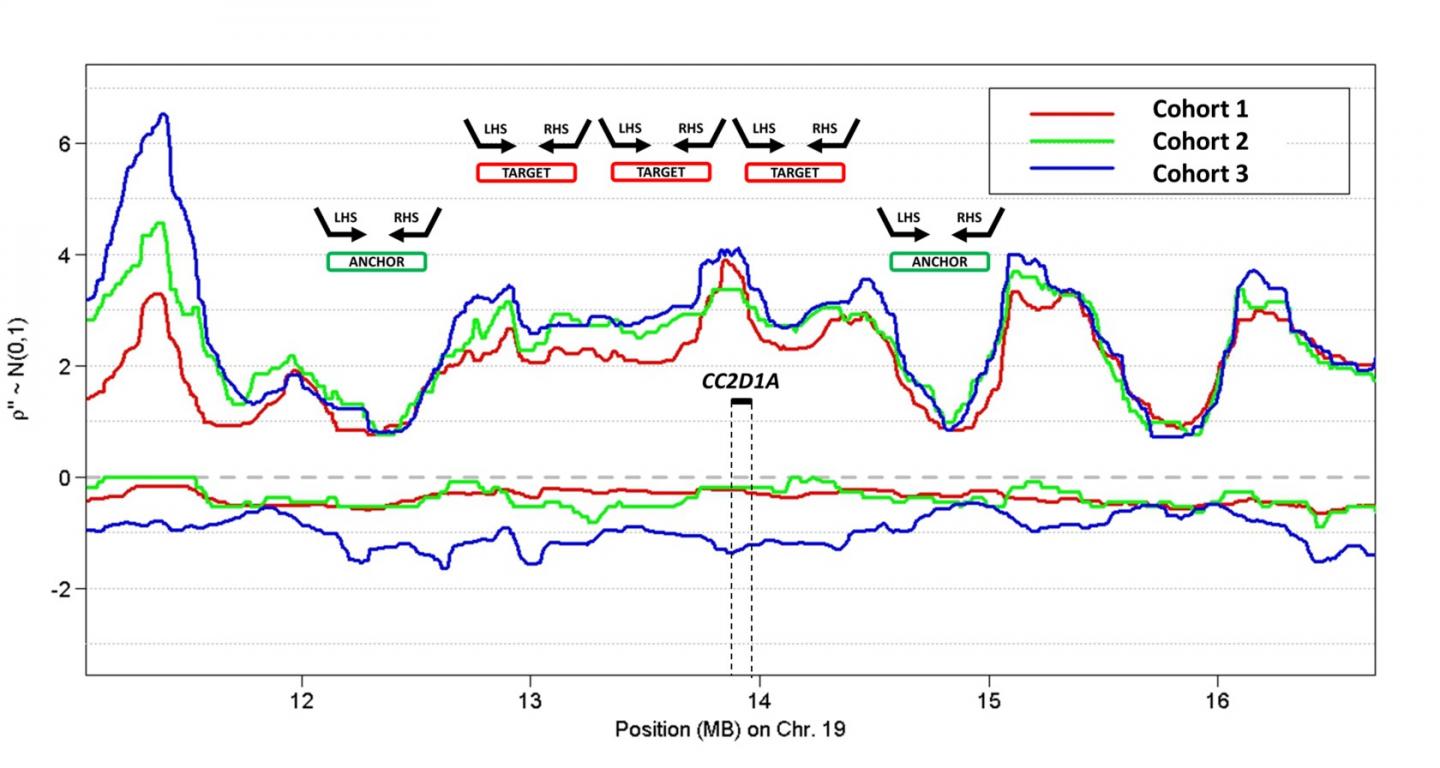
The NG-CNA assay is a targeted amplification sequencing technique that is able to analyze 902 genomic sites belonging to 194 genomic regions. Compared to array comparative genomic hybridization array (CGH), NG-CNA can process samples faster and decrease the cost per sample. “For example, with NG-CNA the cost of DNA extraction, library preparation, and sequencing reagents can be $20 to $40 per sample, compared to nearly $1000 for whole genome sequencing,” said Dr. Ostrer.
In fact, “massively multiplexed assays, like the NG-CNA assay, provide an entry into personalized medicine applications at a fraction of the cost of traditional whole genome sequencing approaches,” added first author Viacheslav Fofanov, PhD, of the School of Informatics, Computing, and Cyber Systems, Northern Arizona University, Flagstaff, AZ, USA.
Another practical advantage of NG-CNA is that the results are easier to decipher than whole genome sequencing. The new assay allows hundreds to thousands of samples to be processed in a single run, with a typical turn-around time of 36 hours. Samples evaluated with the NG-CNA assay also require less data storage than whole genome sequencing. “This allows our approach to move from large reference laboratories to smaller, more resource-constrained independent laboratories as needed,” added Dr. Ostrer.
A further benefit of the NG-CNA assay is that it can process smaller amounts of material (as low as 12.5 ng) than required by other techniques, allowing cell lines, surgical samples, and biopsies to be analyzed. The CNA approach also provides a single platform onto which other sequencing tests, such as companion diagnostic tests, can be incorporated.
In previous work, the researchers developed the metastatic potential score (MPS) as an indicator of metastatic potential, using data from other measurement techniques. They found the MPS to be highly predictive of prostate cancer, triple negative breast cancer, and lung adenocarcinoma metastases. In the current investigation, NG-CNA assay data were used to compute the MPS in 70 prostate cancer surgical research samples with known clinical outcomes, and the results were highly correlated with that of the Oncoscan CNV assay. In a separate group, clinical and analytical validity was found between surgical samples and matched biopsies run exclusively on the NG-CNA platform. An MPS threshold of 0.99 delineated high risk from low risk tumors.
“We believe the addition of the NG-CNA assay onto a standard cancer gene testing platform will augment personalized medicine by identifying aggressive tumors and genetic mutations that are predictors of response to targeted therapies,” said Dr. Ostrer.
###
Media Contact
Eileen Leahy
[email protected]
732-238-3628
Related Journal Article
http://dx.




