Genetically engineered immune cells can drive an aggressive type of leukaemia into retreat, a small clinical trial suggests.
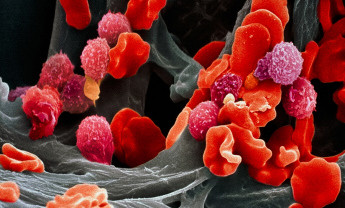
The results of the trial — done in five patients with acute lymphoblastic leukaemia — are published in Science Translational Medicine1 and represent the latest success for a ‘fringe’ therapy in which a type of immune cell called T cells are extracted from a patient, genetically modified, and then reinfused back. In this case, the T cells were engineered to express a receptor for a protein on other immune cells, known as B cells, found in both healthy and cancerous tissue.
When reintroduced into the patients, the tricked T cells quickly homed in on their targets. “All of our patients very rapidly cleared the tumour,” says Michel Sadelain, a researcher at the Memorial Sloan-Kettering Cancer Center in New York and an author of the study. The treatment “worked much faster than we thought”.
The technique has already shown promise against chronic leukaemia, but there were doubts about whether it could take on the faster-growing acute lymphoblastic leukaemia, a tenacious disease that kills more than 60% of those afflicted.
Carl June, an immunologist at the University of Pennsylvania in Philadelphia and a pioneer in engineering T cells to fight cancer, says that he is surprised that the method worked so well against such a swift-growing cancer. The next step, he says, is to move the technique out of the ‘boutique’ academic cancer centres that developed it and into multicentre clinical trials.
“What needs to be done is to convince oncologists and cancer biologists that this new kind of immunotherapy can work,” he says.
Extra hope
Oncologist Renier Brentjens, also at Memorial Sloan-Kettering Cancer Center, remembers the day that he had to tell one of the patients in the trial that the weeks of high-dose chemotherapy the 58-year-old man had endured had not worked after all. “It was painful to have that conversation,” says Brentjens. “He tells me now it was the worst news he has ever heard in his life.”
Another month in the hospital on intensive chemotherapy drugs did nothing to help. By the time the man started the trial, 70% of his bone marrow was tumour.
Brentjens, Sadelain and their colleagues then extracted T cells from the patient and engineered them to express a ‘chimeric antigen receptor’, or CAR, that would target cells expressing a protein called CD19. Because CD19 is found on both healthy and cancerous B cells, the engineered T cells were unable to discriminate between the two. However, patients can live without B cells.
By two weeks after the procedure, the patient was showing signs of improvement. The treatment had driven his cancer into remission — as it did for the other four patients in the trial — so he became eligible for a bone-marrow transplant. A hundred days later, he is doing well, says Brentjens. Four of the five patients were well enough to receive transplants; the remaining patient relapsed and was ineligible.
Pharmaceutical firms have tended to be wary of the CAR technique because it is technically challenging, must be personalized to the patient and faces an untested path to regulatory approval, says Steven Rosenberg, head of the tumour immunology section at the National Cancer Institute in Bethesda, Maryland.
But this seems to be changing. Rosenberg points to a collaboration formed in August last year between June’s group and the drug giant Novartis, as well as the launch of several small CAR-focused biotechnology firms. And Sadelein says that he is an investigator on a trial with the Dana-Farber Cancer Institute in Boston, Massachusetts, to test whether the technique can be exported to other treatment centers, among other outcomes.
Brentjens, meanwhile, is happy to have his patients in fighting spirits again. “You see these people at their lowest low emotionally as well as physically,” he says. “And now you can tell they’re in better shape because they’re making fun of your tie again.”
Story source:
The above story is reprinted from materials provided by Nature News.