A new technique invented at MIT can precisely measure the growth of many individual cells simultaneously. The advance holds promise for fast drug tests, offers new insights into growth variation across single cells within larger populations, and helps track the dynamic growth of cells to changing environmental conditions.
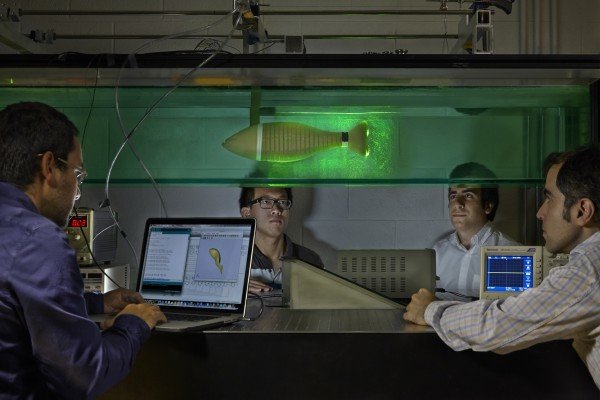
The technique, described in a paper published in Nature Biotechnology, uses an array of suspended microchannel resonators (SMR), a type of microfluidic device that measures the mass of individual cells as they flow through tiny channels. A novel design has increased throughput of the device by nearly two orders of magnitude, while retaining precision. The paper’s senior author, MIT professor Scott Manalis, and other researchers have been developing SMRs for nearly a decade.
In the new study, the researchers used the device to observe the effects of antibiotics and antimicrobial peptides on bacteria, and to pinpoint growth variations of single cells among populations, which has important clinical applications. Slower-growing bacteria, for instance, can sometimes be more resistant to antibiotics and may lead to recurrent infections.
“The device provides new insights into how cells grow and respond to drugs,” says Manalis, the Andrew (1956) and Erna Viterbi Professor in the MIT departments of Biological Engineering and Mechanical Engineering and a member of the Koch Institute for Integrative Cancer Research.
The paper’s lead authors are Nathan Cermak, a recent PhD graduate from MIT’s Computational and Systems Biology Program, and Selim Olcum, a research scientist at the Koch Institute. There are 13 other co-authors on the paper, from the Koch Institute, MIT’s Microsystems Technology Laboratory, the Dana-Farber Cancer Institute, Innovative Micro Technology, and CEA LETI in France.
Array of hope
Manalis and his colleagues first developed the SMR in 2007 and have since introduced multiple innovations for different purposes, including to track single cell growth over time, measure cell density, weigh cell-secreted nanovesicles, and, most recently, measure the short-term growth response of cells in changing nutrient conditions.
All of these techniques have relied on a crucial scheme: One fluid-filled microchannel is etched in a tiny silicon cantilever sensor that vibrates inside a vacuum cavity. When a cell enters the cantilever, it slightly alters the sensor’s vibration frequency, and this signal can be used to determine the cell’s weight. To measure a cell’s growth rate, Manalis and colleagues could pass an individual cell through the channel repeatedly, back and forth, over a period of about 20 minutes. During that time, a cell can accumulate mass that is measurable by the SMR. But while the SMR weighs cells 10 to 100 times more accurately than any other method, it has been limited to one cell at a time, meaning it could take many hours, or even days, to measure enough cells.
The key to the new technology was designing and controlling an array of 10 to 12 cantilever sensors that act like weigh stations, recording the mass of a cell as it flows through the postage-stamp-sized device. Between each sensor are winding “delay channels,” each about five centimeters in length, through which the cells flow for about two minutes, giving them time to grow before reaching the next sensor. Whenever one cell exits a sensor, another cell can enter, increasing the device’s throughput. Results show the mass of each cell at each sensor, graphing the extent to which they’ve grown or shrunk.
In the study, the researchers were able to measure about 60 mammalian cells and 150 bacteria per hour, compared to single SMRs, which measured only a few cells in that time. “Being able to rapidly measure the full distribution of growth rates shows us both how typical cells are behaving, and also lets us detect outliers — which was previously very difficult with limited throughput or precision,” Cermak says.
One comparable method for measuring masses of many individual cells simultaneously is called quantitative phase microscopy (QPM), which calculates the dry mass of cells by measuring their optical thickness. Unlike the SMR-based approach, QPM can be used on cells that grow adhered to surfaces. However, the SMR-based approach is significantly more precise. “We can reliably resolve changes of less than one-tenth of a percent of a cancer cell’s mass in about 20 minutes. This precision is proving to be essential for many of the clinical applications that we’re pursuing,” Olcum says.
New drug-testing capabilities
In one experiment using the device, the researchers observed the effects of an antibiotic, called kanamycin, on E. coli. Kanamycin inhibits protein synthesis in bacteria, eventually stopping their growth and killing the cells.
Traditional antibiotic tests require growing a culture of bacteria, which could take a day or more. Using the new device, within an hour the researchers recorded a change in rate in which the cells accumulate mass. The reduced recording time is critical in testing drugs against bacterial infections in clinical settings, Manalis says: “In some cases, having a rapid test for selecting an antibiotic can make an important difference in the survival of a patient.”
Similarly, the researchers used the device to observe the effects of an antimicrobial peptide called CM15, a relatively new protein-based candidate for fighting bacteria. Such candidates are increasingly important as bacteria strains become resistant to common antibiotics. CM15 makes microscopic holes in bacteria cell walls, such that the cell’s contents gradually leak out, eventually killing the cell. However, because only the mass of the cell changes and not its size, the effects may be missed by traditional microscopy techniques. Indeed, the researchers observed the E. coli cells rapidly losing mass immediately following exposure to CM15. Such results could lend validation to the peptide and other novel drugs by providing some insight into the mechanism, Manalis says.
The researchers are currently working with members of the Dana Farber Cancer Institute, through the MIT/DFCI Bridge program, to determine if the device could be used to predict patient response to therapy by weighing tumor cells in the presence of anticancer drugs.
###
The research was sponsored, in part, by the U.S. Army Research Office, the MIT/DFCI Bridge program, the National Science Foundation, and the National Cancer Institute.
Media Contact
Abby Abazorius
[email protected]
617-253-2709
@MIT
http://web.mit.edu/newsoffice
The post Device rapidly measures growth of single cells simultaneously appeared first on Scienmag.