Almost every biological process involves sensing the presence of a certain chemical. Finely tuned over millions of years of evolution, the body’s different receptors are shaped to accept certain target chemicals. When they bind, the receptors tell their host cells to produce nerve impulses, regulate metabolism, defend the body against invaders, or myriad other actions depending on the cell, receptor, and chemical type.
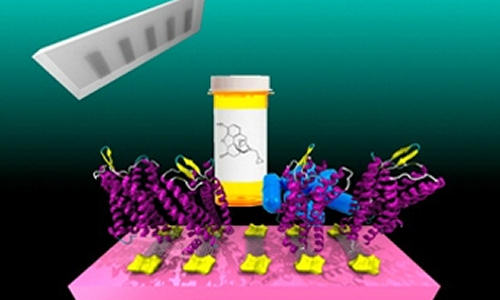
An illustration of the researchers’ devices. Ribbons of graphene (silver) are mounted on circuitry (gold), which can read out a response when the attached receptor proteins (purple) bind to a target molecule.
Now, Penn researchers created an artificial chemical sensor based on one of the human body’s most important receptors—one that is critical in the action of painkillers and anesthetics. In these devices, the receptors’ activation produces an electrical response rather than a biochemical one, allowing that response to be read out by a computer.
By attaching a modified version of this mu-opioid receptor to strips of graphene, researchers have shown a way to mass-produce devices that could be useful in drug development and a variety of diagnostic tests.
Their study combines recent advances from several disciplines and labs around campus, including those of A.T. Charlie Johnson, director of Penn’s Nano/Bio Interface Center and professor of physics in Penn Arts & Sciences, Renyu Liu, assistant professor of anesthesiology in the Perelman School of Medicine, and Jeffery Saven, professor of chemistry in Penn Arts & Sciences.
Saven’s and Liu’s groups have used computational techniques to redesign the mu-opioid receptor to make it easier to use in research. In its natural state, the receptor is not water soluble, making many common experimental techniques impossible. Worse, proteins like this receptor would normally be grown en masse using genetically engineered bacteria, but parts of the natural mu-opioid receptor are toxic to the E. coli used in this method.
After Saven and Liu addressed these problems with the redesigned receptor, they saw that it might be useful to Johnson, who had previously published a study on attaching a similar receptor protein to carbon nanotubes. In that case, the protein was difficult to grow genetically, and needed to include additional biological structures from the receptors’ natural membranes in order to remain stable.
Saven and Liu’s computationally redesigned protein, however, could be readily grown and attached directly to graphene, opening up the possibility of mass-producing biosensor devices that utilize these receptors.
“This is the kind of project that the Penn campus makes possible,” Saven says. “Even with the Medical School across the street and the Physics Department nearby, I don’t think we’d be as close collaborators without the Nano/Bio Interface Center supporting us.”
With Saven and Liu providing a version of the receptor that could stably bind to sheets of graphene, Johnson’s team refined the manufacturing process. Starting with a sheet of graphene about 6 inches wide by 12 inches long, the researchers separated them into ribbons an inch long and about 50 microns across. Then, they placed the ribbons on top of pre-fabricated circuitry.
Once attached to the ribbons, the opioid receptors are able produce changes in the surrounding graphene’s electrical properties whenever they bind to their target. Those changes produce electrical signals that are transmitted to a computer via neighboring electrodes, each set representing a separate device.
“We can measure each device individually and average the results, which greatly reduces the noise,” Johnson says. “Or you could imagine attaching 10 different kinds of receptors to 20 devices each, all on the same chip, if you wanted to test for multiple chemicals at once.”
In the researcher’s experiment, they tested their devices’ ability to detect the concentration of naltrexone, a drug used in alcohol and opioid addiction treatment because it binds to—and blocks—the natural opioid receptors that produce the narcotic effects patients seek.
“It’s not clear whether the receptors on the devices are as selective as they are in the biological context,” Saven says, “as the ones on your cells that can tell the difference between an agonist, like morphine, and an antagonist, like naltrexone, which binds to the receptor but does nothing. By working with the receptor-functionalized graphene devices, however, not only can we make better diagnostic tools, but we can also potentially get a better understanding of how the bimolecular system actually works in the body.”
Liu notes that many novel opioids have been developed over the centuries, however, none of them has achieved potent analgesic effects without notorious side effects, including devastating addiction and respiratory depression.
“This novel tool could potentially aid the development of new opioids that minimize these side effects,” he says.
Wherever these devices find applications, they are a testament to the potential usefulness of the Nobel-prize winning material on which they are based.
“Graphene gives us an advantage,” Johnson says, “in that its uniformity allows us to make 192 devices on a one inch chip, all at the same time. There are still a number of things we need to work out, but this is definitely a pathway to making these devices in large quantities.”
Story Source:
The above story is based on materials provided by University of Pennsylvania.