Regenerative medicine researchers at Wake Forest Baptist Medical Center have addressed a major challenge in the quest to build replacement kidneys in the lab. Working with human-sized pig kidneys, the scientists developed the most successful method to date to keep blood vessels in the new organs open and flowing with blood. The work is reported in journal Technology.
Anthony Atala, M.D., director and professor at the Wake Forest Institute for Regenerative Medicine
“Until now, lab-built kidneys have been rodent-sized and have functioned for only one or two hours after transplantation because blood clots developed,” said Anthony Atala, M.D., director and professor at the Wake Forest Institute for Regenerative Medicine and a senior author on the study. “In our proof-of-concept study, the vessels in a human-sized pig kidney remained open during a four-hour testing period. We are now conducting a longer-term study to determine how long flow can be maintained.”
If proven successful, the new method to more effectively coat the vessels with cells (endothelial) that keep blood flowing smoothly, could potentially be applied to other complex organs that scientists are working to engineer, including the liver and pancreas.
The current research is part of a long-term project to use pig kidneys to make support structures known as “scaffolds” that could potentially be used to build replacement kidneys for human patients with end-stage renal disease. Scientists first remove all animal cells from the organ – leaving only the organ structure or “skeleton.” A patient’s own cells would then be placed in the scaffold, making an organ that the patient theoretically would not reject.
The cell removal process leaves behind an intact network of blood vessels that can potentially supply the new organ with oxygen. However, scientists working to repopulate kidney scaffolds with cells have had problems coating the vessels and severe clotting has generally occurred within a few hours after transplantation.
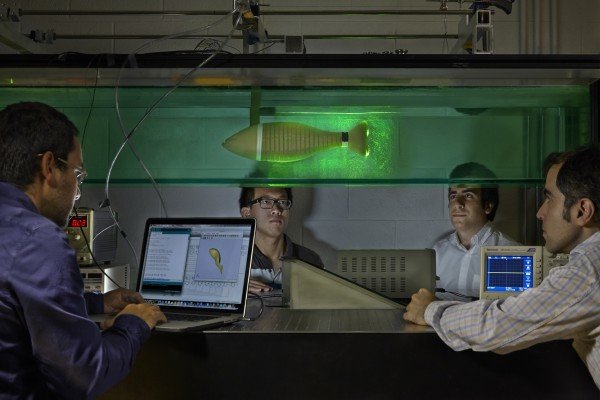
The Wake Forest Baptist scientists took a two-pronged approach to address this problem. First, they evaluated four different methods of introducing new cells into the main vessels of the kidney scaffold. They found that a combination of infusing cells with a syringe, followed by a period of pumping cells through the vessels at increasing flow rates, was most effective.
Next, the research team coated the scaffold’s vessels with an antibody designed to make them more “sticky” and to bind endothelial cells. Laboratory and imaging studies — as well as tests of blood flow in the lab – showed that cell coverage of the vessels was sufficient to support blood flow through the entire kidney scaffold.
The final test of the dual-approach was implanting the scaffolds in pigs weighing 90 to 110 pounds. During a four-hour testing period, the vessels remained open.
“Our cell seeding method, combined with the antibody, improves the attachment of cells to the vessel wall and prevents the cells from being detached when blood flow is initiated,” said In Kap Ko, Ph.D., lead author and instructor in regenerative medicine at Wake Forest Baptist.
The scientists said a long-term examination is necessary to sufficiently conclude that blood clotting is prevented when endothelial cells are attached to the vessels.
The scientists said if the new method is proven successful in the long-term, the research brings them an important step closer to the day when replacement kidneys can be built in the lab.
“The results are a promising indicator that it is possible to produce a fully functional vascular system that can deliver nutrients and oxygen to engineered kidneys, as well as other engineered organs,” said Ko.
Using pig kidneys as scaffolds for human patients has several advantages, including that the organs are similar in size and that pig heart valves – removed of cells – have safety been used in patients for more than three decades.
Story Source:
The above story is based on materials provided by Wake Forest Baptist Medical Center.