Researchers develop a compact artificial lung that could be worn in a fanny pack and received a $3.4 million federal grant to help make it happen.
Photo Credits:Trib Total Media
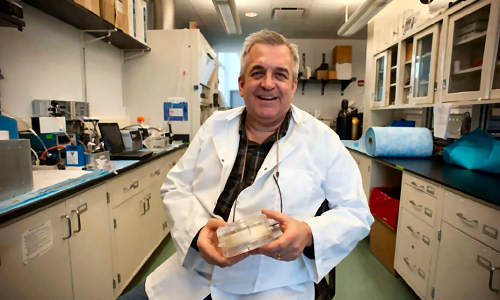
William Federspiel, a professor of bioengineering at the University of Pittsburgh, is leading a team that will use the grant from the National Institutes of Health, announced Tuesday, to replace technologies that keep those awaiting lung transplants or recovering from acute, chronic-lung failure bedridden and tethered to cumbersome machines to breathe.
“Lots and lots of people die of respiratory failure each day. A truly effective artificial lung would be a very important medical advance,” said Dr. Norman H. Edelman, chief medical officer for the American Lung Association, who is not involved with the research. “Transplants do work and are successful, but they are hard to come by. So having something to tide a patient over until a transplant would be an important advance.”
Thousands of people need such treatments to recover from lung disease. In the United States alone, experts estimate that 350,000 people a year die of lung disease; 150,000 more require medical care for it.
Federspiel’s team includes scientists and physicians from Pitt, UPMC, Carnegie Mellon University and Mississippi State University. In a laboratory on the South Side, researchers have assembled a small model of the device they hope to perfect.
The Paracorporeal Ambulatory Assist Lung, or PAAL, would remove blood through a plastic tube inserted into a vein, remove carbon dioxide from the blood and inject oxygen into it. The blood would be returned to the body through a second tube.
PAAL, which will weigh 3 to 5 pounds, likely would involve another year or two of development with a medical-device company before it is ready for clinical trial in humans, Federspiel said.
It’s a far cry from cumbersome, stationary machines now used to drain blood from the body, re-oxygenate it and return it to the bloodstream.
“Our wearable lung will allow lung patients to get up and moving within the hospital setting,” Federspiel said.
“Clinical literature indicates if you can get patients off sedation and up moving, you improve recovery from acute lung disease. And if they are a candidate for a lung transplantation, you can improve outcomes because you have healthier patients.”
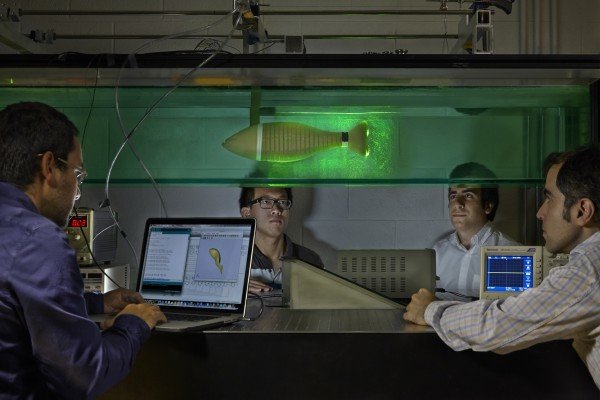
The project takes place as researchers from the University of Maryland test an artificial lung on animals. Federspiel said the Pittsburgh lung would feature a different design, incorporating a spinning component that would mix oxygen in the blood like a spoon that stirs cream into coffee.
Edelman compared the development of a successful compact artificial lung to the device that kept former Vice President Dick Cheney alive while he awaited a heart transplant.
“Something like this could truly improve life for a certain subset of people,” Edelman said.
Story Source:
The above story is based on materials provided by Trib Total Media, Debra Erdley.- via University of Pittsburgh