In recent years, ovarian cancer has remained one of the most challenging malignancies, primarily due to its often late diagnosis and its intricate biological mechanisms. A groundbreaking study conducted by a team of researchers led by Zhao Y., Chen Q., and Li J. has unveiled the involvement of the vascular endothelial generating factor pathway in ovarian cancer. This significant finding, published in the Journal of Ovarian Research, provides new insights into the biology of ovarian tumors and highlights potential avenues for therapeutic intervention. Understanding how this pathway operates in the realm of ovarian cancer may hold the key to unlocking novel treatment strategies that could dramatically improve patient outcomes.
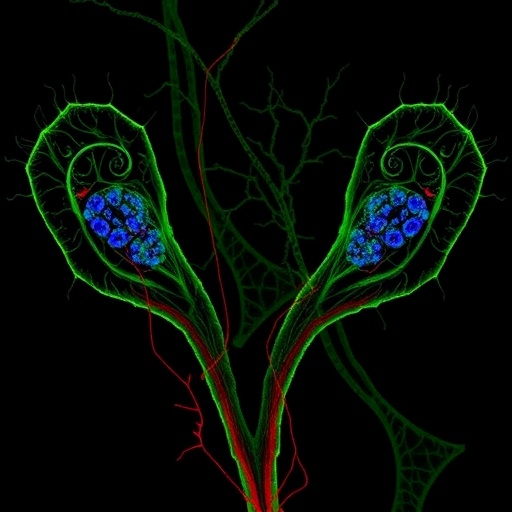
The vascular endothelial growth factor (VEGF) pathway is known for its fundamental role in angiogenesis, the process by which new blood vessels form from existing ones. In cancer biology, the activation of this pathway is often associated with tumor growth and metastasis. The study by Zhao et al. meticulously elucidates how the VEGF pathway operates in ovarian cancer. By profiling various cell lines and tumor samples, the researchers demonstrated a pronounced expression of VEGF isoforms, which are critical in promoting angiogenesis within the tumor microenvironment. Their work reveals a complex network where the interplay of different cells influences the ability of ovarian cancer to thrive and disseminate.
One of the notable aspects of this research is the identification of specific molecular markers associated with the activation of the VEGF pathway in ovarian cancer. The study presents a plethora of data indicating upregulated expressions of key components, such as VEGF-A, VEGF-C, and their receptors in samples obtained from ovarian cancer patients. These findings suggest that the VEGF pathway is not only a facilitator of vascular growth but also plays an essential role in tumor aggressiveness. The implications of these results are far-reaching; understanding these markers could pave the way for the development of targeted therapies aimed at disrupting the pro-angiogenic signaling that supports tumor advancement.
Moreover, the authors delve into the ramifications of the VEGF pathway on the immune landscape surrounding ovarian tumors. This research illustrates that the activation of the VEGF pathway does not merely aid tumor growth but also has immunosuppressive consequences. By examining tumor-infiltrating lymphocytes, Zhao and colleagues reported a significant reduction in cytotoxic T cell activities in the presence of elevated VEGF levels. This interplay between angiogenesis and immune modulation illustrates the dual role of the VEGF pathway in sustaining tumor survival and evading immune detection, ultimately complicating treatment efforts.
In light of these discoveries, the authors propose that interrupting the VEGF signaling pathway could potentially reinvigorate the immune response against ovarian tumors. The study reviews various existing anti-angiogenic therapies and evaluates their limitations when used as standalone treatments. There has been considerable interest in employing these agents in conjunction with immune checkpoint inhibitors, and Zhao et al. emphasize this combinatorial approach as a promising direction for future research. The hope is that by simultaneously targeting angiogenesis and enhancing immune function, more effective treatment regimens can be developed for patients battling ovarian cancer.
Furthermore, the research underscores the need for personalized medicine in the context of ovarian cancer treatment. By establishing a clearer connection between the VEGF pathway and tumor behavior, the authors argue that specific stratifications of patients based on biomarker expression could lead to more tailored therapeutic strategies. This personalized approach could enhance patient responses and minimize the adverse effects typically associated with more generalized treatment methodologies.
The implications of this research extend beyond the laboratory, resonating within clinical settings. It is critical to note that the findings not only advance our understanding of ovarian cancer biology but also may influence future diagnostic protocols. Screening for VEGF pathway-associated biomarkers could emerge as a routine part of the diagnostic process, aiding in early detection and potentially guiding treatment decisions. The combination of improved diagnostics with innovative therapeutic approaches has the potential to alter the treatment landscape for ovarian cancer radically.
While the study presents groundbreaking insights, it also highlights significant questions that remain unanswered in the field of ovarian cancer research. For instance, the precise mechanisms by which VEGF signaling leads to immune evasion are still obscure. Future studies are warranted to dissect the underlying pathways further and explore the possibility of additional molecular players within the tumor microenvironment. Continued investigation into the cooperative roles of different angiogenic factors and immune cells will be essential in building a comprehensive understanding of this multifaceted disease.
In summary, the research conducted by Zhao, Chen, Li, and their collaborators presents compelling evidence of the critical role played by the vascular endothelial generating factor pathway in ovarian cancer. Their findings not only enhance our understanding of the disease’s biology but also open new avenues for targeted therapies that have the potential to improve patient survival rates significantly. The combination of anti-angiogenic agents with immunotherapy seems to represent a promising future direction in the fight against ovarian cancer, emphasizing the importance of integrating cutting-edge research with clinical practices. This roadmap to tackling ovarian cancer hinges on collaborative efforts in both basic and translational research, paving the way for breakthroughs that could one day lead to curing this devastating disease.
This research primes us to think critically about how angiogenic pathways can be strategically manipulated to alter the course of cancer treatment. By continuing to investigate the interplay between VEGF signaling and other biological factors involved in tumorigenesis, researchers may unearth novel strategies that could shift the paradigm of care for ovarian cancer patients. The continuing evolution of our understanding in this domain promises to yield substantial health benefits and quality-of-life improvements for those facing this formidable disease.
As the field progresses, fostering collaborations among researchers, clinicians, and pharmaceutical companies will be crucial in bringing these novel insights from the bench to the bedside. The hope is that with sustained efforts to explore the vascular endothelial generating factor pathway and its implications, we may one day witness a significant enhancement in the prognosis for ovarian cancer patients, transforming a historically grim outlook into one of renewed hope and tangible recovery.
Subject of Research: Vascular endothelial generating factor pathway in ovarian cancer
Article Title: Vascular endothelial generating factor pathway in ovarian cancer
Article References:
Zhao, Y., Chen, Q., Li, J. et al. Vascular endothelial generating factor pathway in ovarian cancer.
J Ovarian Res 18, 272 (2025). https://doi.org/10.1186/s13048-025-01864-3
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13048-025-01864-3
Keywords: ovarian cancer, vascular endothelial growth factor, angiogenesis, immunotherapy, personalized medicine
Tags: angiogenesis in cancerbiological mechanisms of ovarian tumorscancer metastasis mechanismsgroundbreaking cancer studieslate diagnosis of ovarian cancerovarian cancer researchpatient outcomes in cancer treatmenttherapeutic interventions for ovarian cancertumor microenvironment dynamicsunderstanding ovarian cancer biologyvascular endothelial growth factor pathwayVEGF isoforms in tumors