In the ongoing battle against head and neck cancer, a novel molecular pathway has emerged as a promising focal point for therapeutic intervention. Recent research highlights the HIF1A-UCA1-PTBP3 axis as a critical driver of tumor progression and metastasis, offering new insights into the underlying mechanisms of this aggressive disease. This revelation paves the way for potential therapies aimed at disrupting this axis, thereby impeding cancer growth and spread.
Long non-coding RNAs (lncRNAs), once deemed mere genomic byproducts, have now captured the spotlight for their multifaceted regulatory functions in gene expression. Among them, the urothelial cancer-associated 1 (UCA1) lncRNA has gained particular attention due to its involvement in various cancers, including bladder, colon, stomach, lung, and breast malignancies. The recent study extends this list by implicating UCA1 in head and neck cancers, especially hypopharyngeal carcinoma (HPC), a subtype notorious for its late detection and poor prognosis.
HPC poses a significant clinical challenge due to its aggressive nature and the high likelihood of relapse and metastatic dissemination, even after curative treatment. Its molecular underpinnings have remained elusive, hampering the development of targeted therapies. The upregulation of UCA1 in HPC patients correlates with disease severity, yet the mechanistic pathways through which UCA1 influences tumor behavior were, until now, poorly understood.
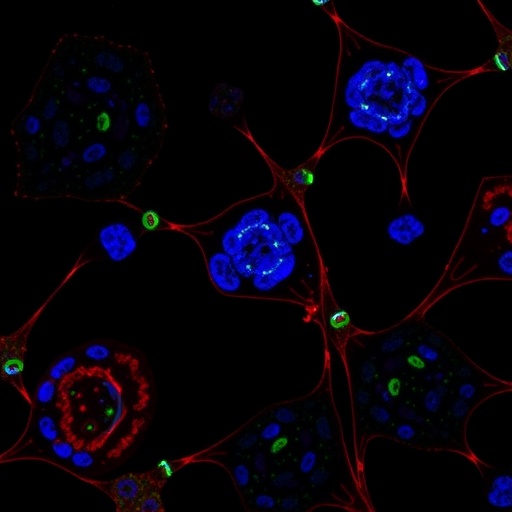
A multidisciplinary research team employed both genetic silencing and ectopic expression techniques to dissect the functional consequences of UCA1 dysregulation in head and neck cancer cell lines. By modulating UCA1 levels, they observed notable effects on cellular behaviors critical to cancer progression, such as proliferation, migration, invasion, and colony formation. These granular in vitro studies laid the groundwork for understanding UCA1’s dualistic role within the tumor microenvironment.
Interestingly, increasing UCA1 expression resulted in enhanced cell migration and invasion capabilities but concurrently led to reduced cell proliferation rates. This paradoxical effect suggests a complex regulatory network at play, potentially involving the modulation of epithelial-mesenchymal transition (EMT) processes. The research identified hallmark changes in both epithelial and mesenchymal markers, indicative of an incomplete EMT state that may facilitate cancer cell dissemination while maintaining viability.
The converse was true when UCA1 was depleted, with treated cells showing diminished motility and invasive potential, underscoring UCA1’s pro-metastatic function. Extending their findings into in vivo models, researchers utilized xenograft systems, confirming that UCA1 depletion significantly impairs tumor growth and notably reduces lymph node metastasis—one of the deadliest aspects of head and neck cancer progression.
At a molecular level, UCA1 was predominantly localized within the nucleus, where it engages in direct interactions with polypyrimidine tract binding protein 3 (PTBP3), an RNA-binding protein implicated in post-transcriptional gene regulation. This interaction was elucidated through RNA pulldown assays followed by mass spectrometry, revealing the physical and functional interplay pivotal for modulating cancer cell behavior.
Manipulating PTBP3 expression demonstrated a compelling reversal of UCA1-induced cellular phenotypes. Overexpression of PTBP3 reinstated the migratory and invasive capabilities of UCA1-depleted cells, underscoring its role as a downstream effector. This finding positions PTBP3 as a critical mediator coupling UCA1’s regulatory functions to phenotypic outcomes relevant to cancer metastasis.
Further exploration revealed that UCA1 expression is sensitive to hypoxic conditions, a hallmark of the tumor microenvironment notorious for fostering aggressive cancer traits. Hypoxia inducible factor 1-alpha (HIF1A), a master regulator of cellular responses to low oxygen levels, was identified as a partially responsible upstream activator of UCA1 transcription. This linkage situates UCA1 within the hypoxia-driven signaling cascade that fuels tumor adaptation and survival.
Moreover, the study demonstrated UCA1’s capability to modulate key signaling molecules such as cyclin D1 and p21, which are pivotal for cell cycle regulation, as well as influencing Smad2 phosphorylation—a central event in the TGF-β signaling pathway. By mimicking TGF-β effects, UCA1 enhances trans-endothelial migration, a process critical for tumor cells to breach vascular barriers and establish distant metastases.
Collectively, these findings reveal a complex signaling axis whereby hypoxia through HIF1A induction elevates nuclear UCA1 levels, which in turn binds PTBP3 to drive phenotypic changes favoring migration, invasion, and metastatic spread. This axis not only elucidates a novel molecular framework for head and neck cancer progression but also identifies multiple targets for therapeutic intervention to hinder tumor dissemination.
Given the dismal prognosis associated with advanced head and neck cancers, targeting the HIF1A-UCA1-PTBP3 axis represents a beacon of hope for developing effective treatments. Therapeutic strategies that disrupt this axis could simultaneously impair metastatic potential and improve patient survival outcomes, marking a paradigm shift in cancer therapeutics.
Future research endeavors are warranted to translate these molecular insights into clinical therapies, including the design of small molecules or antisense oligonucleotides targeting UCA1 or PTBP3. Additionally, investigating the broader implications of this axis across other cancer types may reveal universal principles of tumor biology and metastasis.
The discovery of this intricate molecular pathway further exemplifies the critical role of lncRNAs in cancer biology, challenging previous notions of their functional insignificance. It also reinforces the need for integrated research approaches that encompass genetic, biochemical, and animal model studies to unravel the complexities of cancer progression.
In summary, the identification and characterization of the HIF1A-UCA1-PTBP3 axis significantly advances our understanding of head and neck cancer metastasis. By bridging hypoxia-induced transcriptional regulation with RNA-protein interactions that modulate cellular migratory behavior, this axis offers a novel and promising target for therapeutic innovation in an area of unmet medical need.
Subject of Research: Mechanistic investigation of the HIF1A-UCA1-PTBP3 molecular axis in the progression and metastasis of head and neck cancer.
Article Title: Targeting the HIF1A-UCA1-PTBP3 axis: a potential therapeutic strategy for head and neck cancer.
Article References:
Sim, L.CL., Kuo, YZ., Cheng, TC. et al. Targeting the HIF1A-UCA1-PTBP3 axis: a potential therapeutic strategy for head and neck cancer. BMC Cancer 25, 1536 (2025). https://doi.org/10.1186/s12885-025-15020-z
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-15020-z
Tags: aggressive cancer subtypescancer progression mechanismscancer relapse and prognosisemerging cancer treatment targetshead and neck cancer treatmentHIF1A-UCA1-PTBP3 cancer therapyhypopharyngeal carcinoma researchlncRNAs and gene expressionlong non-coding RNAs in cancermetastatic cancer pathwaystargeted cancer therapy strategiesUCA1 lncRNA in tumors