Low-cost biosensor test developed by Penn Medicine could extend reliable COVID-19 testing to remote and disadvantaged areas
Credit: Penn Medicine
PHILADELPHIA–A low-cost, rapid diagnostic test for COVID-19 developed by Penn Medicine provides COVID-19 results within four minutes with 90 percent accuracy. A paper published this week in Matter details the fast and inexpensive diagnostic test, called RAPID 1.0 (Real-time Accurate Portable Impedimetric Detection prototype 1.0). Compared to existing methods for COVID-19 detection, RAPID is inexpensive and highly scalable, allowing the production of millions of units per week.
Despite the urgency of the pandemic, most available methods for COVID-19 testing use RT-PCR–reverse transcription polymerase chain reaction–to detect SARS-CoV-2. Though effective, the technique requires large laboratory space and trained workers to employ. These tests are also costly, they run a risk of cross-contamination, and can take hours or days to provide results.
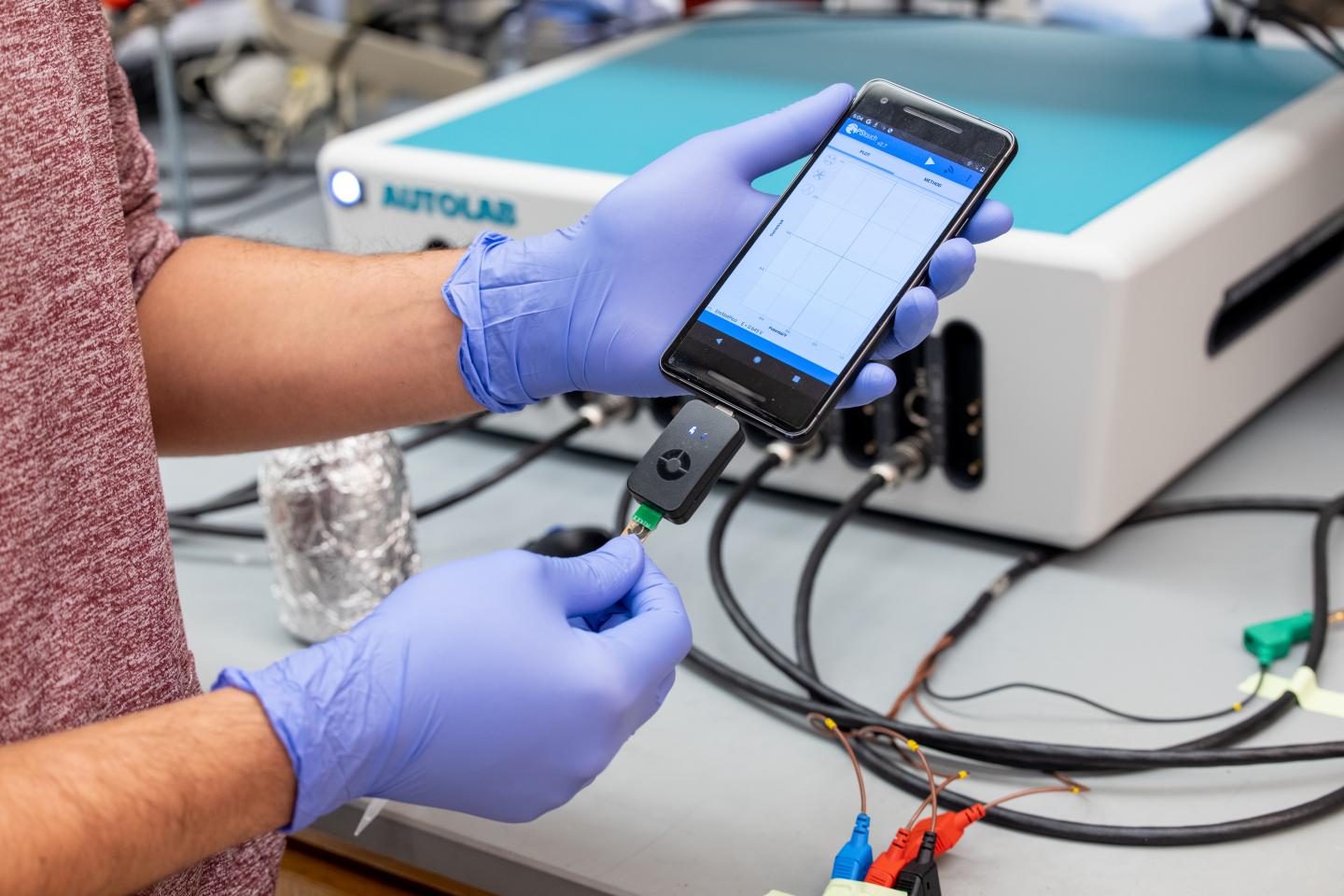
RAPID was developed by a team led by César de la Fuente, PhD, a Presidential Assistant Professor in Psychiatry, Microbiology, Chemical and Biomolecular Engineering, and Bioengineering, to quickly and accurately detect the virus while remaining cheap enough to be widely accessible. An electrode printed using a screen printer–thousands of which can be printed in a day at very low cost–can detect the virus in nasal swab or saliva samples. The results can be read on a benchtop instrument or on a smartphone.
“Prior to the pandemic, our lab was working on diagnostics for bacterial infections. But then, COVID-19 hit. We felt a responsibility to use our expertise to help–and the diagnostic space was ripe for improvements,” de la Fuente said. “We feel strongly about the health inequities witnessed during the pandemic, with testing access and the vaccine rollout, for example. We believe inexpensive diagnostic tests like RAPID could help bridge some of those gaps.”
The RAPID technology uses electrochemical impedance spectroscopy (EIS), which transforms the binding event between the SARS-CoV-2 viral spike protein and its receptor in the human body, the protein ACE2 (which provides the entry point for the coronavirus to hook into and infect human cells), into an electrical signal that clinicians and technicians can detect. That signal allows the test to discriminate between infected and healthy human samples. The signal can be read through a desktop instrument or a smartphone.
The team assessed the performance of RAPID using both COVID-19 positive and negative clinical samples from the Hospital of the University of Pennsylvania, including samples of the highly contagious UK B117 variant. In blinded tests, they analyzed 139 nasal swab samples–109 of which were COVID-19 positive and 30 COVID-19 negative, as determined by standard RT-PCR clinical assessments. The team also analyzed 50 saliva samples from patients. For the nasal swab samples, RAPID was 87.1 percent accurate. For saliva samples, RAPID was 90 percent accurate.
RAPID provides results in four minutes, which is faster than most methods currently available for diagnosing COVID-19. For example, serological tests can take around 15 to 20 minutes, and they are about 60 to 70 percent accurate. In addition, RAPID is able to detect COVID-19 at extremely low concentrations (1.16 PFU mL), which corresponds to a viral load that correlates with the initial stages of COVID-19 (about two to three days after onset of symptoms). This is beneficial for detecting individuals at the earliest stages of infection, allowing for rapid care and the potential decrease of further viral spread.
“Quick and reliable tests like RAPID allow for high-frequency testing, which can help identify asymptomatic individuals who, once they learn they are infected, will stay home and decrease spread. We envision this type of test being able to be used at high-populated locations such as schools, airports, stadiums, companies–or even in one’s own home,” said first author Marcelo Der Torossian Torres, PhD, a postdoctoral researcher at Penn.
Importantly, the technology is affordable and scalable. Each test, which can be performed at room temperature, costs $4.67 to produce. Additionally, the electrodes used in the test can be quickly mass-produced using commercially available screen-printers to print the circuit board (named eChip). One laboratory-sized unit is able to produce 35,000 electrodes daily (about 1.05 million per month).
The team also constructed an electrode for RAPID composed of filter paper, which is a more accessible and inexpensive material. Named ePAD, the researchers demonstrated the applicability of ePAD for RAPID in a portable method, connected to a smart device, which may enable further scale and on-demand testing capabilities at the point-of-care.
“Having low-cost tests which are quick and easy to read extends testing to not only people who can afford it, but to remote or disadvantaged areas,” de la Fuente said.
De la Fuente lab’s research focuses primarily on developing technologies that help understand, prevent, and treat infectious diseases. Though RAPID was developed as a COVID-19 test, the technology can be used to detect other viruses and diagnose a variety of diseases such as the flu or sexually transmitted diseases.
###
The research was supported by the Nemirovsky Prize, the Dean’s Innovation Fund from the Perelman School of Medicine at the University of Pennsylvania, Brazil’s Coordination for the Improvement of Higher Education Personnel (88887.479793/2020-00), São Paulo Research Foundation (2018/08782-1), FAEPEX/PRP/UNICAMP (3374/19), and Brazil’s National Council for Scientific and Technological Development (438828/2018-6, 401256/2020-0). A provisional patent application has been filed on the technology described in this manuscript (Invention Disclosure 21-9515).
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation’s first medical school) and the University of Pennsylvania Health System, which together form a $8.9 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report’s survey of research-oriented medical schools. The School is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $496 million awarded in the 2020 fiscal year.
The University of Pennsylvania Health System’s patient care facilities include: the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center–which are recognized as one of the nation’s top “Honor Roll” hospitals by U.S. News & World Report–Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; and Pennsylvania Hospital, the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is powered by a talented and dedicated workforce of more than 44,000 people. The organization also has alliances with top community health systems across both Southeastern Pennsylvania and Southern New Jersey, creating more options for patients no matter where they live.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2020, Penn Medicine provided more than $563 million to benefit our community.
Media Contact
Hannah Messinger
[email protected]
Related Journal Article
http://dx.