Fralin Biomedical Research Institute scientist earns $2.8 million grant to study cerebrovascular changes during healthy and Alzheimer’s aging
Credit: Virginia Tech
Scientists often focus on abnormal accumulations of proteins called plaques in the brain in efforts to find a treatment for Alzheimer’s disease. But the effects of these plaques have not been clear.
Virginia Tech scientists are exploring how these deposits may be degrading the brain’s vascular system, which circulates blood, providing oxygen and glucose to the cells responsible for perception, movement, thinking, and memory, while also eliminating metabolic waste.
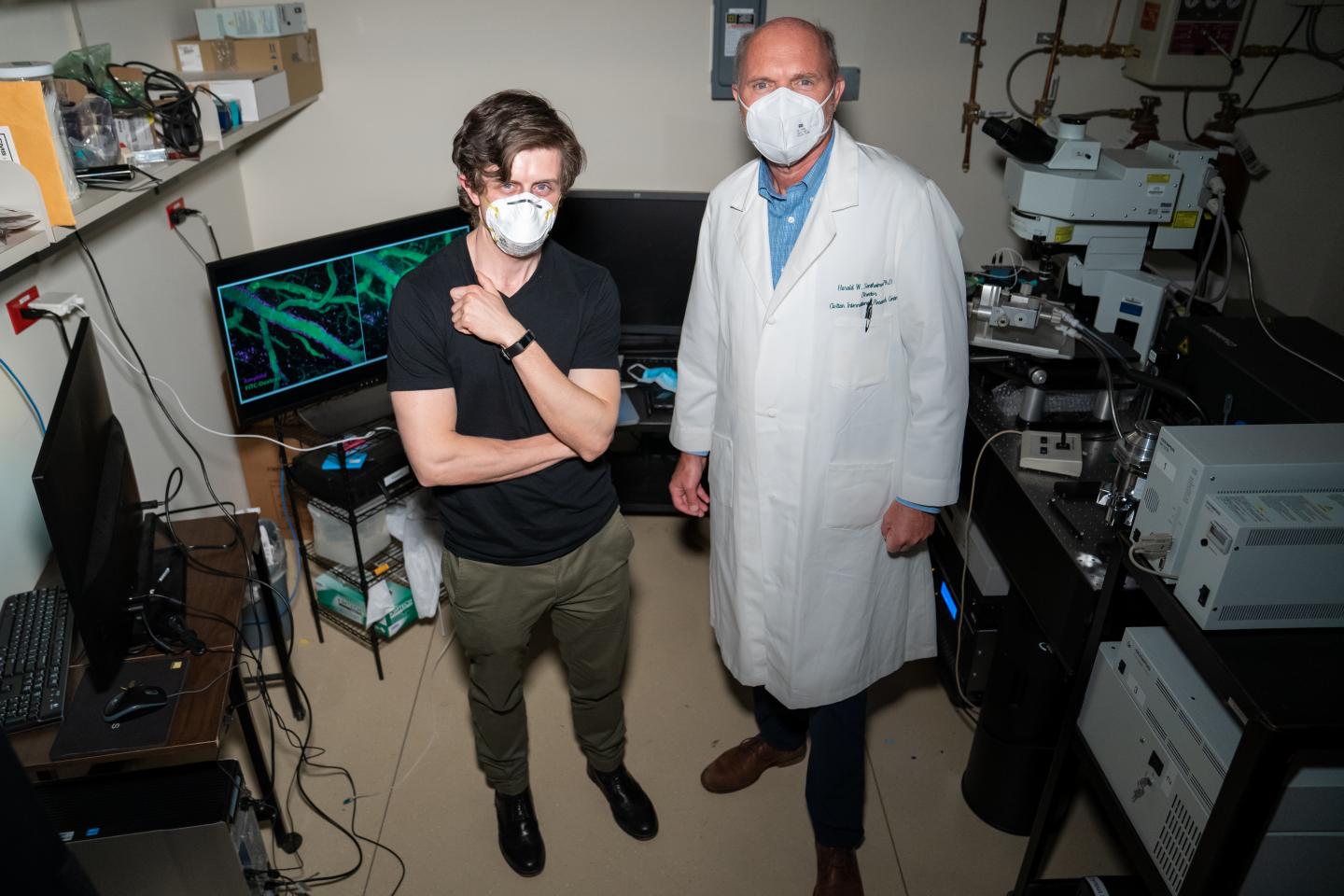
Supported by a new, five-year, $2.8 million National Institutes of Health grant awarded to Harald Sontheimer, a glial neurobiologist at the Fralin Biomedical Research Institute at VTC, scientists are probing changes caused by aging in the circulatory system in the normal brain and Alzheimer’s disease brain.
Alzheimer’s disease is an irreversible, progressive brain disorder that slowly destroys memory and thinking skills, and, eventually, the ability to carry out tasks, according to the National Institute on Aging. As the disease progresses, once-healthy neurons stop functioning, lose connections with other neurons, and die.
But instead of the ailing neurons, researchers with the Fralin Biomedical Research Institute Center for Glial Biology in Health, Disease and Cancer are focused on an abundant group of brain cells known for maintaining optimal brain health.
They are concentrating on a type of glial cell called astrocytes, which may become damaged by the amyloid plaques and unable to support the brain’s circulatory system and, ultimately, the neurons.
“We’re saying that the amyloid is not primarily toxic to neurons or the vascular system, but to the astrocytes,” said Sontheimer, who is a professor at the Fralin Biomedical Research Institute and the School of Neuroscience in the Virginia Tech College of Science. “As the amyloid impairs the astrocytes and their ability to regulate blood flow, the brain is starved of oxygen and energy, and therefore, neurons gradually die. In people we see conditions of memory loss and dementia. This whole decline is accelerated by the presence of amyloid in Alzheimer’s disease.”
In a healthy brain, microscopic blood vessels are surrounded by specialized smooth muscle cells that contract or relax to constrict or dilate the vessels to regulate the appropriate amount of blood flow to a given brain region based on demand. Astrocytes interact with blood vessels through specialized processes called “endfeet,” which cover almost the entire surface of the blood vessels.
“It was long believed that neurons somehow regulated this blood flow,” said Sontheimer, who is the director of the Center for Glial Biology in Health, Disease, and Cancer. “It turns out that astrocytes actually sense neuronal activity and release molecules to dilate these blood vessels to allow more blood, glucose, and oxygen to get to regions where they are most needed. Everyone had assumed that the amyloid itself is impairing the blood vessels, but it’s actually impairing the astrocytes.”
As an additional consequence, the blood vessel becomes leaky, representing a weakening of the blood brain barrier, which protects the brain from circulating toxins and other threats.
Under the grant, awarded by the National Institute of Aging, researchers at the glial biology center are studying a mouse model of a genetic form of Alzheimer’s disease — a rare type that is passed along in families that accounts for less than 5 percent of Alzheimer’s — and mice with a condition similar to what occurs in the presence amyloid plaque. Furthermore, scientists will compare normal aging with aging with Alzheimer’s-like conditions.
“As a control, we would like to look at what occurs during aging alone,” Sontheimer said. “We want to know at what point in time some of these normal processes break down naturally with aging and to what extent those declines may that be accelerated by Alzheimer’s.”
The scientists will isolate astrocytes in mice as they age from three months to two years in both the normal aging and Alzheimer’s aging.
With Michelle Olsen, an associate professor in the School of Neuroscience in the College of Science and affiliated with the research institute’s Center for Glial Biology in Health, Disease, and Cancer, the scientists will pinpoint genes and proteins specifically in astrocytes that are changing to cause negative effects.
“The hope is we’ll discover something completely unsuspected — a protein or a signaling pathway that no one had thought about — that could then be potentially targeted to develop a glia-centered therapy for Alzheimer’s disease,” Sontheimer said.
Symptoms of Alzheimer’s disease most often appear when people are in their mid-60s or older, although the rare familial form can appear at younger ages. Estimates vary, but experts suggest that more than 5.5 million Americans, most of them age 65 or older, may have dementia caused by Alzheimer’s.
“We certainly have the approach and the tools to understand glia and their potential contribution to blood vessel demise and Alzheimer’s disease,” said Tre Mills, a fourth-year student in Virginia Tech’s translational biology, medicine, and health graduate program, who is working on the project in the Sontheimer laboratory.
“If we can understand what’s happening in the beginning stages of the disease, we could prohibit the late stage phenomena, increase the health span, and either slow or stop the progression of Alzheimer’s altogether,” Mills said. “I really think we’re homing in on that mid-stage of people’s lives to prevent or slow down the progression of disease — and that would be phenomenal.”
###
Media Contact
John Pastor
[email protected]
Original Source
https:/