Because viral infections can be controlled by T-cells, the body’s infection-fighting white blood cells, the Children’s National Hospital first-in-humans Phase 1 dose escalation trial aimed to determine the safety of…
view more
Tailored T-cells specially designed to combat a half dozen viruses are safe and may be effective in preventing and treating multiple viral infections, according to research led by Children’s National Hospital faculty.
Catherine Bollard, M.B.Ch.B., M.D., director of the Center for Cancer and Immunology Research at Children’s National and the study’s senior author, presented the teams’ findings Nov. 8, 2019, during a second-annual symposium jointly held by Children’s National and the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH). Children’s National and NIAID formed a research partnership in 2017 to develop and conduct collaborative clinical research studies focused on young children with allergic, immunologic, infectious and inflammatory diseases. Each year, they co-host a symposium to exchange their latest research findings.
According to the NIH, more than 200 forms of primary immune deficiency diseases impact about 500,000 people in the U.S. These rare, genetic diseases so impair the person’s immune system that they experience repeated and sometimes rare infections that can be life threatening. After a hematopoietic stem cell transplantation, brand new stem cells can rebuild the person’s missing or impaired immune system. However, during the window in which the immune system rebuilds, patients can be vulnerable to a host of viral infections.
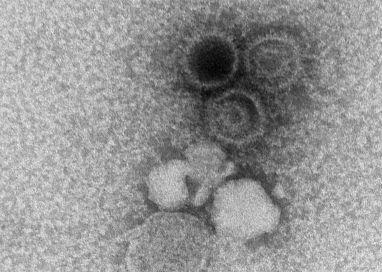
Because viral infections can be controlled by T-cells, the body’s infection-fighting white blood cells, the Children’s National first-in-humans Phase 1 dose escalation trial aimed to determine the safety of T-cells with antiviral activity against a half dozen opportunistic viruses: adenovirus, BK virus, cytomegalovirus (CMV), Epstein-Barr virus (EBV), Human Herpesvirus 6 and human parainfluenza-3 (HPIV3).
Eight patients received the hexa-valent, virus-specific T-cells after their stem cell transplants:
- Three patients were treated for active CMV, and the T-cells resolved their viremia.
- Two patients treated for active BK virus had complete symptom resolution, while one had hemorrhagic cystitis resolved but had fluctuating viral loads in their blood and urine.
- Of two patients treated prophylactically, one developed EBV viremia that was treated with rituximab.
Two additional patients received the T-cell treatments under expanded access for emergency treatment, one for disseminated adenoviremia and the other for HPIV3 pneumonia. While these critically ill patients had partial clinical improvement, they were being treated with steroids which may have dampened their antiviral responses.
“These preliminary results show that hexaviral-specific, virus-specific T-cells are safe and may be effective in preventing and treating multiple viral infections,” says Michael Keller, M.D., a pediatric immunologist at Children’s National and the lead study author. “Of note, enzyme-linked immune absorbent spot assays showed evidence of antiviral T-cell activity by three months post infusion in three of four patients who could be evaluated and expansion was detectable in two patients.”
###
In addition to Drs. Bollard and Keller, additional study authors include Katherine Harris M.D.; Patrick J. Hanley Ph.D., assistant research professor in the Center for Cancer and Immunology; Allistair Abraham, M.D., a blood and marrow transplantation specialist; Blachy J. Dávila Saldaña, M.D., Division of Blood and Marrow Transplantation; Nan Zhang Ph.D.; Gelina Sani BS; Haili Lang MS; Richard Childs M.D.; and Richard Jones M.D.
Children’s National-NIAID 2019 symposium presentations
“Welcome and introduction”
H. Clifford Lane, M.D., director of NIAID’s Division of Clinical Research
“Lessons and benefits from collaboration between the NIH and a free-standing children’s hospital”
Marshall L. Summar, M.D., director, Rare Disease Institute, Children’s National
“The hereditary disorders of PropionylCoA and Cobalamin Metabolism – past, present and future”
Charles P. Venditti, M.D., Ph.D., National Human Genome Research Institute Collaboration
“The road(s) to genetic precision therapeutics in pediatric neuromuscular disease: opportunities and challenges”
Carsten G. Bönnemann, M.D., National Institute of Neurological Disorders and Stroke
“Genomic diagnostics in immunologic diseases”
Helen Su, M.D., Ph.D., National Institute of Allergy and Infectious Diseases
“Update on outcomes of gene therapy clinical trials for X-SCID and X-CGD and plans for future trials”
Harry Malech, M.D., National Institute of Allergy and Infectious Diseases
“Virus-specific T-cell therapies: broadening applicability for PID patients”
Catherine Bollard, M.D., Children’s National
“Using genetic testing to guide therapeutic decisions in Primary Immune Deficiency Disease”
Vanessa Bundy, M.D., Ph.D., Children’s National
Panel discussion moderated by Lisa M. Guay-Woodford, M.D.
Drs. Su, Malech, Bollard and Bundy
Morgan Similuk, S.C.M., NIAID
Maren Chamorro, Parent Advocate
“Underlying mechanisms of pediatric food allergy: focus on B cells
Adora Lin, M.D., Ph.D., Children’s National
“Pediatric Lyme outcomes study – interim update”
Roberta L. DeBiasi, M.D., MS, Children’s National
“Molecular drivers and opportunities in neuroimmune conditions of pediatric onset”
Elizabeth Wells, M.D., Children’s National
Media Contact
Diedtra Henderson
[email protected]
443-610-9826




