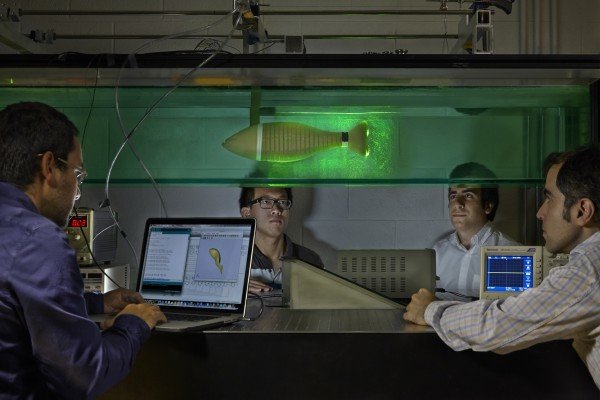
In a scientific first, Harvard Stem Cell Institute scientists have successfully grown the cells that line the blood vessels—called vascular endothelial cells—from human induced pluripotent stem cells (iPSCs), revealing new details about how these cells function. Using a unique approach, the researchers induced the differentiation of specific cell types by generating mechanical forces on the surface of the iPSC-derived endothelium mimicking the flow of blood. For example, cells that felt a stronger “flow” became artery cells, while those that felt a weaker “flow” became vein cells.
“It was especially exciting to us to discover that these cells are basically responding to biomechanical cues,” research leader Guillermo García-Cardena, PhD, an HSCI Affiliated Faculty member, said. “By exposing cells to ‘atheroprone flow,’ we can direct differentiation of these cells into cells that are present in areas of the circulatory system that we know are affected by diseases like atherosclerosis.” García-Cardena is now working on modeling the formation of arterial plaques using human iPSC-derived vascular endothelial cells and identifying potential drugs that might prevent plaque formation.
García-Cardena’s team, which included Harvard School of Engineering and Applied Sciences graduate student William Adams, found that the iPS-derived human endothelial cells display three critical functions carried out by mature endothelium in the body: mounting inflammatory responses, keeping blood from leaking out of the blood vessel, and preventing blood clots.
Based on this information, García-Cardena’s work, published this month in the journal Stem Cell Reports, has another exciting implication—it could potentially reduce, or even eliminate the need for heparin use during kidney dialysis and lung failure treatment—making both markedly safer.
Traditionally, patients undergoing dialysis are treated with heparin, a powerful drug, which prevents the blood from clotting as it’s routed through the dialysis machine. While heparin is quite effective in preventing clotting, because it considerably thins the blood, it can also cause loss of blood, internal bleeding, and interfere with the healing process.
“The iPSC-derived endothelial cells cells beautifully function as an anticoagulant surface,” said García-Cardena, an Associate Professor of Pathology at Harvard Medical School and Brigham and Women’s Hospital. “In the future, we may take a tissue sample from a patient, generate iPSCs, and then cover an extracorporeal device with the patient’s own endothelial cells—so the patient can go home with the device without the need for regular heparin shots.”