UNIGE researchers have developed a cell co-culture platform that can reproduce a patient’s tumour in 3D and test the best treatment combinations for its specific case in just five days
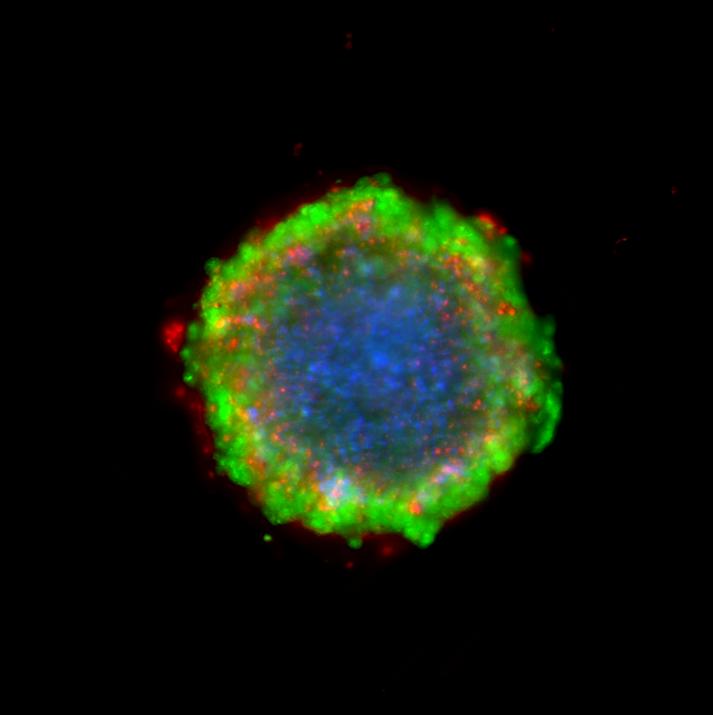
Credit: © UNIGE, Molecular Pharmacology Group
Why doesn’t the same treatment work in the same way for every patient? How can a drug’s performance be optimised without causing side effects due to an excessive dosage? In an attempt to answer these questions, researchers at the University of Geneva (UNIGE), Switzerland, have devised a cell co-culture platform that reproduces a patient’s tumour structure in 3D. The scientists can use it to test several drugs or their combinations at different stages of the tumour’s development. They now need only five days to identify which treatment will be most effective for a particular case, and the combination can then be translated for clinical practice. These results are highly promising for the future of personalised medicine, and you can read all about the outcomes in the journal Scientific Reports.
Colorectal cancer is the third most common form of cancer diagnosed today and the fourth most deadly in the world: 1.4 million people are affected each year, with 700,000 fatalities. A range of treatments is available, including chemotherapy, but the high dosages cause numerous side effects and patients commonly develop resistance. These treatments are currently tested on 2D tumour cell cultures before being administered to patients. “But that doesn’t correspond to reality,» explains Patrycja Nowak-Sliwinska, a professor at the School of Pharmaceutical Sciences at the UNIGE’s Faculty of Science. “Not only does a tumour develop in 3D, but it also contains other types of cells, such as fibroblasts (tissues) and endothelial cells (blood vessels).” As a result, the Geneva-based scientists have built a new platform that uses a patient’s tumour cell lines to recreate the tumour in 3D. It also keeps it alive, so that the impact of the treatments can be analysed during the different stages of its development.
To each patient, his or her own tumour
The team headed by professor Nowak-Sliwinska, in collaboration with groups led by Didier Colin (HUG) and Olivier Dormond (CHUV), selected six cell lines derived from six different patients. The cells were stabilised in a hollow, U-shaped culture plate so that they stayed agglomerated and floated in a cell culture medium optimised to feed the tumour. “The structure can then be organised by itself in 3D and continue its development,” says professor Nowak-Sliwinska. “The three types of cells that make up the tumour carry on interacting with each other, as though they were in the patient’s body.”
Three drugs better than one
The researchers then tested several different combinations of three approved drugs at different developmental stages of the cultured tumours. “Our first observation was that each patient responded differently to the same combination, demonstrating that it’s impossible to reach similar efficacy for each patient with the same treatment. It needs to be considered on a case-by-case basis,” says professor Nowak-Sliwinska. The scientists also found that a low-dose combination of three drugs was much more effective than a high-dose of one drug alone. “Treatment resistance and side effects occur when the dose is too high. Combining several drugs at low doses helps to circumvent this problem and improve treatment responses,” says the professor.
Personalised treatments in five days
The new platform opens the door to personalised medicine. “By extracting a cell line from the patient’s tumour, we can recreate the tumour in 3D on our platform and test the different drug combinations directly on that specific tumour. We can then select the optimal treatment for that particular patient”, continues professor Nowak-Sliwinska. This meticulous work takes five days on average, a short enough time to act quickly against the cancer. “In this instance, we’re interested in colorectal cancer but this platform, which is easy to reproduce, can obviously be used for all kinds of tumours at a relatively low cost,” says Nowak-Sliwinska by way of conclusion.
###
Media Contact
Patrycja Nowak-Sliwinska
[email protected]
Related Journal Article
http://dx.




