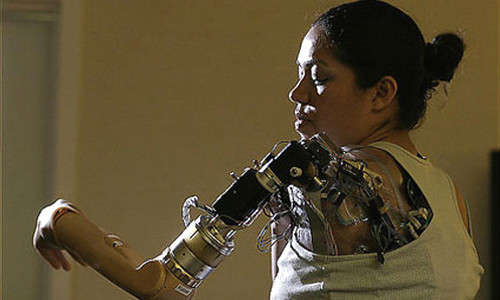
Claudia Mitchell, who lives in Ellicott City, is the fourth person — and first woman — to receive a “bionic” arm, which allows her to control parts of the device by her thoughts alone. The device, designed by physicians and engineers at the Rehabilitation Institute of Chicago, works by detecting the movements of a chest muscle that has been rewired to the stumps of nerves that once went to her now-missing limb.
Mitchell and the first person to get a bionic arm — a power-line technician who lost both arms to a severe electric shock — will demonstrate their prostheses today at a news event in Washington. The Rehabilitation Institute of Chicago is part of a multi-lab effort, funded with nearly $50 million from the Defense Advanced Research Projects Agency (DARPA), to create more useful and natural artificial limbs for amputees.
As of July, 411 members of the military serving in Iraq, and 37 in Afghanistan, have suffered wounds requiring amputation of at least one limb. (How many involved losing arms could not be immediately learned.) Mitchell spent four years in the Marine Corps but did not lose her arm during military service.
Someday she hopes to upgrade to a prosthesis, still under development, that will allow her also to “feel” with an artificial hand. She is ready for it now.
Last summer, surgeons took the first step by rewiring the skin above her left breast so that when the area is stimulated by impulses from the bionic arm, the skin sends a message to the region of her brain that feels “hand.”
Future arms will also be able to perform more complicated motions. She recently spent time at the Chicago hospital trying out a prototype with six motors, not just the three of her current prosthesis. It will theoretically allow her to reach for things over her head.
But even the first-generation device “has changed my life dramatically,” she said. “I use it to help with cooking, for holding a laundry basket, for folding clothes — all kinds of daily tasks.”
For Todd A. Kuiken, 46, a physician and biomedical engineer, this is the latest step in his 20-year effort to make a better artificial arm. Over that time, his laboratory has spent about $3 million on research and development, with more than $2 million provided by the National Institutes of Health.
The particular achievement with Mitchell is that her prosthesis works with her breast intact. With previous versions, surgeons removed some chest tissue so that electrodes in the arm could better detect twitches in the rewired chest muscles. But that would have been particularly disfiguring.
Nevertheless, Kuiken said: “This is very much a prototype device. We have a lot of smoke in this lab. We fry a lot of transistors.”
The bionic arm makes use of several features of the human body that would be impossible to create from scratch. Luckily, a person still has them even after suffering an injury as grievous as the loss of an arm at the shoulder.
One feature is the “motor cortex” of the brain, where cells that control voluntary muscles reside. The millions of nerve cells that “drive” the arm and hand remain after amputation. When an amputee pretends to move his missing hand, those cells fire and send impulses down the spinal cord and out to nerves that terminate at the stump.
Those nerves are huge electrical conduits filled with tens of thousands of fibers carrying a wide assortment of information. Some are motor nerves telling muscles to move. Some are sensory nerves, carrying impulses back from the hand to the brain, where the information will be interpreted as touch, temperature, pressure and pain.
In preparation for the bionic arm, Kuiken and his surgical colleagues first re-create a biological control panel for a hand on the amputee’s chest. They use muscle and skin that can be sacrificed — or, more precisely, hijacked — for that purpose.
They cut the nerves to two chest muscles, the pectoralis and serratus, at a point where those nerves have branched to go to different parts of the muscles, but far “upstream” from the point where the nerves divide into tiny fibers that attach to individual bundles of muscle fiber.
They then sew the stumps of the large nerves that once went to the arm and hand to the cut ends of the chest-muscle nerves. In the same operation, the nerves carrying sensation from the skin over the pectoral muscle are also sewn into the arm nerves.
Over several months, the arm nerves grow down the sheaths of the motor fibers and attach to the muscles. (Interestingly, the amputee assists this process by mentally “exercising” the missing hand, which helps promote a firm nerve-muscle connection.) Simultaneously, the sensory nerves grow down the sensory sheaths and into the skin.
If all goes well, a person is left with chest muscles that twitch in different places in response to such thoughts as “bend the wrist back,” “move the thumb” and “clench the fingers.” The person also ends up with a patch of skin about the width of a baseball that, when stroked, warmed or pricked, feels like a hand rather than part of the chest.
The bionic arm makes use of this feat of anatomical alchemy.
The prosthesis is strapped onto the shoulder stump and torso in a way that positions electrodes over the regions of the chest muscles that are responding to different “hand instructions.” Those electrodes, in turn, are wired to a computer and then on to motors in the forearm and hand of the device.
When the amputee tells the fingers to close, the designated part of the pectoral or serratus muscle twitches and the electrode over it detects the signal, activating the appropriate motor.
In the future, electrodes in the hand will send touch signals up the arm to the chest skin, which will send them on to the brain, where they will be perceived as sensation.
Story Source:
The above story is reprinted from materials provided by Washington Post