Credit: Travis Goldsmith/West Virginia University
The novel coronavirus pandemic has nearly exhausted stockpiles of medical gear in the United States. Personal protective equipment, like masks, serve as a first-line defense for medical professionals with a front row seat to COVID-19.
Coming to the aid of those doctors and nurses is a team of scientists from West Virginia University and the National Institute for Occupational Safety and Health, which has developed two alternative face coverings that are as effective at blocking novel coronavirus than those highly-coveted N95 masks.
You may even have some of the materials to make them: a home furnace filter and a 3D printer.
When COVID-19 began to creep into West Virginia, health officials and the state National Guard started scrambling for solutions to safeguard first responders, healthcare providers and patients affected by a lack of PPE.
They sought out expertise in WVU’s Center for Inhalation Toxicology led by Timothy Nurkiewicz. iTOX includes the state-of-the-art WVU Inhalation Facility where researchers can test the effects of inhaled particles, even simulated COVID-19 droplets.
Nurkiewicz and his team concluded that air filter material from home furnaces – you know, the ones you forget to change every three months – can effectively obstruct coronavirus particles.
“HVAC furnace filters – especially the higher quality filters that remove allergens and dust mites – can perform well in blocking COVID-19,” said Nurkiewicz, chair of Physiology and Pharmacology at the WVU School of Medicine. “We can layer that up and use it with publicly-available 3D designs for respirator masks that would cover your face. That combination provides significant protection to anyone exposed to COVID-19 droplets.”
Travis Goldsmith, iTOX senior research engineer, started the project by exploring ways to rapidly test unconventional filter materials. iTox worked in conjunction with Veronica Cyphert, Julie O’Neil and Dr. Robert Gerbo, of WVU Occupational Medicine, to identify that the air filter material in a 3D-printed mask worked quite well.
Dr. Matthew Dietz, from WVU Orthopaedics, brought in additional 3D-printing expertise and added common window/door gaskets to the mask. This addition earned the mask the designation of “pass” for clinical fit testing performed by Occupational Medicine.
The team has forwarded those recommendations to the West Virginia National Guard, which is in the process of producing those masks. The National Guard has a network of printers that are currently being utilized, Nurkiewicz said.
For the second successful alternative, Nurkiewicz’s team developed an adapter that can be 3D-printed and modified to universally fit any face mask. Goldsmith and Kevin Engels, of Physiology and Pharmacology, first developed a prototype. Oxana and Mark Tseytlin from WVU Biochemistry and Walter McKinney and Erik Sinsel from NIOSH in Morgantown worked quickly to develop the prototype into a 3D-printed product and try it out on a CPAP mask. The team discovered that it effectively blocked simulated coronavirus droplets from seeping through.
Nurkiewicz said the design templates will be made available free to the public in the coming weeks as the team refines the files.
“Without the expertise of West Virginia University’s researchers and expert faculty, we wouldn’t be in a position to move forward with our network of academic institutions, community and technical colleges, public and private industries who are able to 3D-print these tested designs to meet the ever-growing need for PPE in our state,” said Maj. Gen. James Hoyer, adjutant general of the West Virginia National Guard. “This collaboration underscores the importance of building strong partnerships among academia and government agencies to develop innovative solutions to the most pressing issues facing our populace, including our current fight against COVID-19 in the Mountain State.”
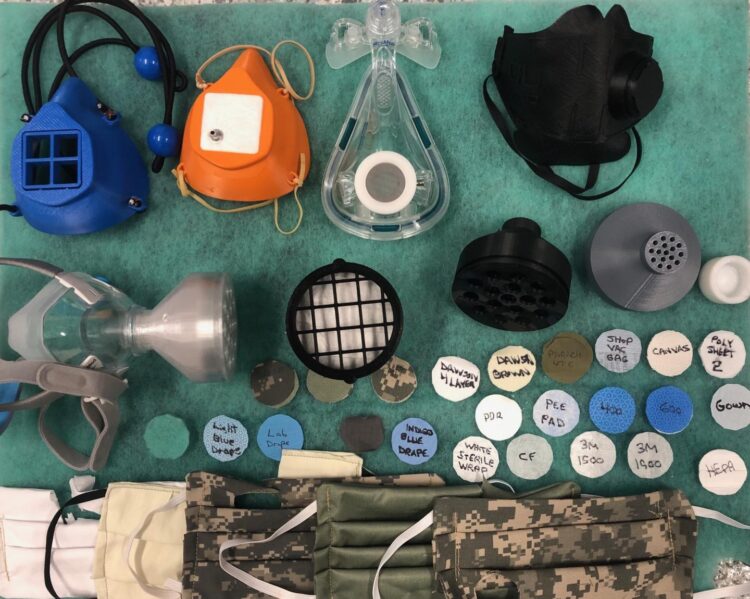
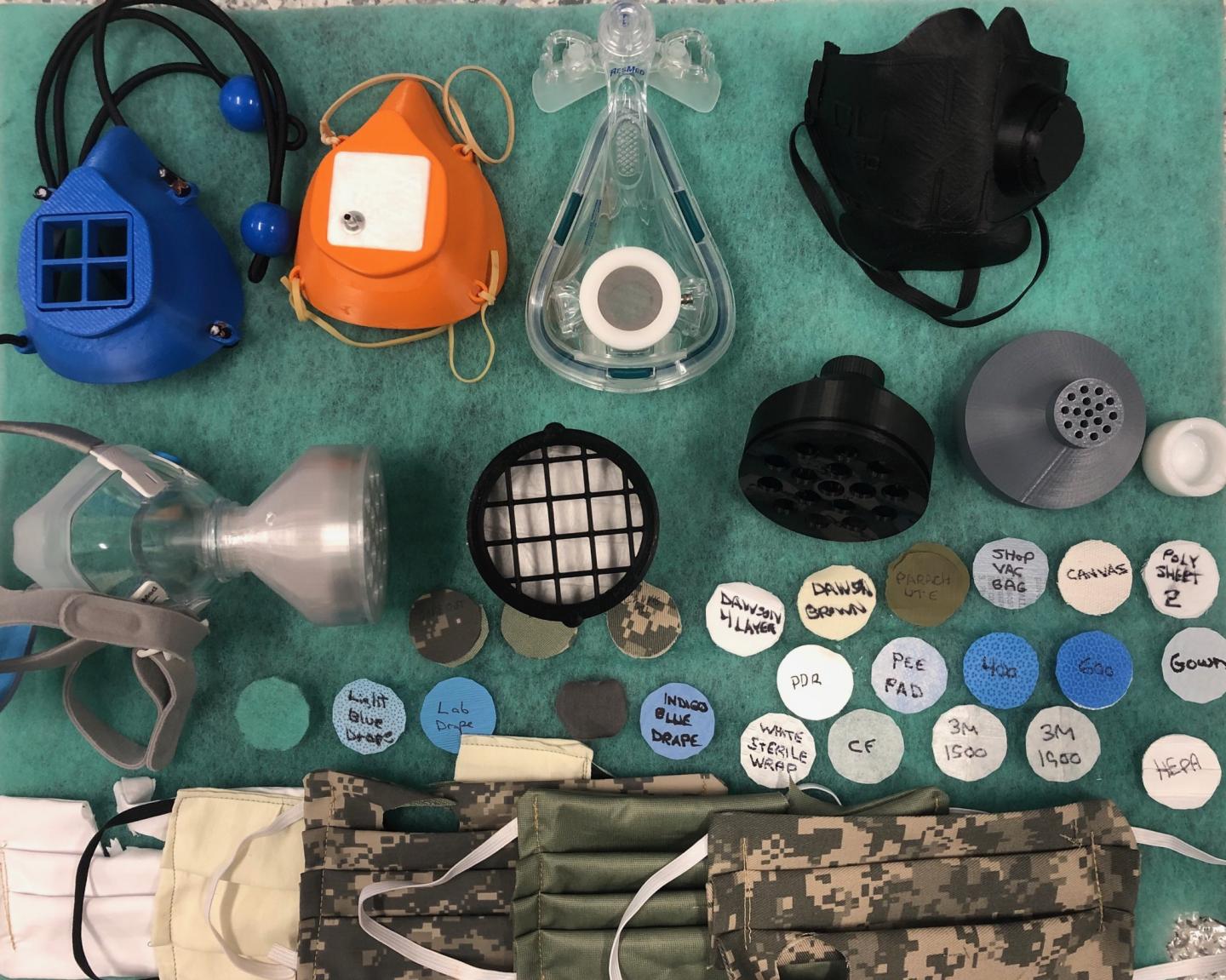
Overall, the team tested more than 20 materials and mask designs. As health professionals prepare for an expected peak in novel coronavirus cases in West Virginia in the coming weeks, Nurkiewicz’s team is monitoring the local levels of PPE and is ready to assist if needed.
The WVU Inhalation Facility measures, identifies and discovers how particles we breathe affect our health. It provides researchers with real-time monitoring capabilities, while the many types of respirable particles it can accommodate during simultaneous experiments make it a standout internationally.
“We have the capacity to generate artificial atmospheres of droplets and particles and can assess the size distribution of aerosols. Normally we assess the impact of their inhalation on the cardiopulmonary and reproductive systems” Nurkiewicz said. “Now, we are determining whether or not a filter is performing a barrier function. Over the course of the past few weeks, we’ve tested pretty much everything.”
Inside the Inhalation Facility, Nurkiewicz’s team conducts aerosol generation exposures, which uses ultrasound pulses to move particles and dusts without physical contact. Researchers have previously used the iTOX facility to study nanomaterials and inhalable particles from e-cigarettes, auto emissions and military burn pits.
“Necessity is the mother of invention,” Nurkiewicz said in reflecting on the last few weeks. “We dream and come up with a bunch of crazy ideas but working with the military has really been enlightening and rewarding. They are an awesome group of people, and we are very fortunate to have their service.”
Nurkiewicz said the research would not have been possible without a dedicated effort from a diverse team of experts coming together as one.
Media Contact
Jake Stump
[email protected]
Original Source
https:/