Credit: USZ
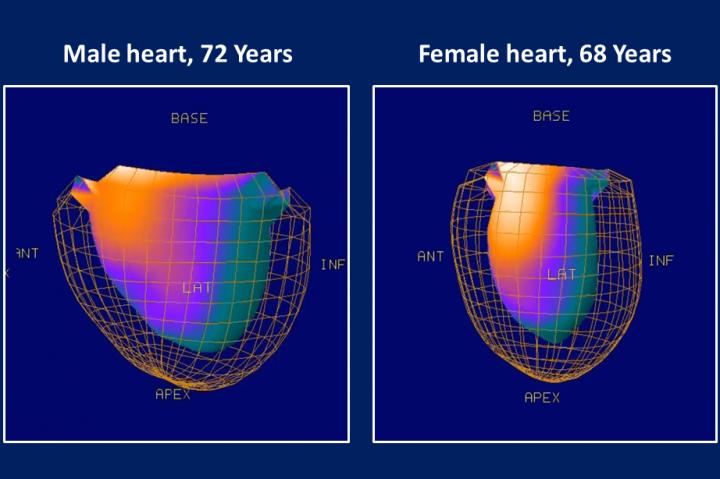
At present, a focus on males in basic research and clinical trials means that models of disease are also based on men. Symptoms and disease progression in male patients are therefore considered the standard, while disease manifestations that are usually observed in women are judged “atypical”. Cardiology is a typical example of a medical field where treatment concepts have been geared to one specific gender, although presentation and outcomes of many cardiovascular conditions are different in women and men. Indeed, a heart attack is still considered a typical male’s disease, although women encounter a heart attack just as often – but on average 10 years later than men.
“It is known that women with an acute myocardial infarction report more often unspecific symptoms and, consequently, experience higher patient and system delays”. says Prof. Cathérine Gebhard, cardiologist at the University Hospital Zurich and program director for the new CAS in “Sex- and Gender-Specific Medicine”. The opposite scenario also occurs, but much more rarely, explains Gebhard. “Management strategies for “typical” female conditions such as osteoporosis are derived from predominantly female populations and the disease is widely unrecognized and undertreated in men.”
There are also sex and gender differences in the efficacy of pharmaceuticals: although it is known that drug metabolism is different in the female body, women remain largely underrepresented in most clinical trials. Accordingly, the latest reports from the US Food and Drug Administration (FDA) for the period from 2004 to 2013 reveal that side effects occur 50% more frequently in women than in men.
The precision medicine of the future should address each individual’s specific needs, says Gebhard: “Considering sex and gender differences in patient care is an important first step.”
Putting insights about sex- and gender-specific differences into practice
Our understanding of sex- and gender-specific aspects of medicine increases every year, aided by several thousand research publications. However, their translation into clinical practice is very slow. The inclusion of gender differences in basic medical training is still in the early stages. Therefore, Prof. Daniel Candinas, Vice-Rector for Research at the University of Bern and Clinic Director of the University Clinic for Visceral Surgery and Medicine at the Inselspital Bern, and Prof. Beatrice Beck Schimmer, Vice President Medicine (UMZH) at the University of Zurich, have launched the CAS continuing education program in “Sex- and Gender-Specific Medicine”, the first of its kind in Switzerland.
Unique in Europe
As of May 2020, eleven modules teaching sex- and gender-specific aspects in various medical disciplines will be available. These will be taught by both national and international experts, include research topics, discuss the latest evidence and touch on the issue of knowledge gaps. In addition to the full CAS, it is also possible to attend individual modules. The further education program is aimed at medical professionals and specialists in related fields who want to broaden their knowledge of sex- and gender-specific differences in medicine and base their practices on the latest research. Organizationally, this CAS is provided by the University of Bern, but modules will be offered both at the universities of Bern and Zurich.
“The CAS in Sex- and Gender-Specific Medicine is a comprehensive study program that should directly benefit the well-being of patients. It is the only one of its kind in Europe” says Prof. Daniel Candinas. “We are looking forward to this collaboration.” says Prof. Beatrice Beck Schimmer. “The universities of Bern and Zurich combine their established expertise to bring insights about sex- and gender-specific medicine into Swiss practices and hospitals.”
###
Media Contact
Daniel Candinas
[email protected]
41-316-322-404
Original Source
https:/




