Credit: Department of Ophthalmology and Visual Science,TMDU
Researchers from Tokyo Medical and Dental University (TMDU) report a case of frosted branch angiitis in a woman presenting years after being treated for leukemia-lymphoma with allogeneic human stem cell transplant.
Tokyo, Japan – Leukemias and lymphomas are life-threatening malignancies affecting white blood cells and the immune system; fortunately, radiotherapy and chemotherapy, combined with stem cell therapy, can improve survival significantly. Now, Japanese researchers report one such patient who presented with an intriguing and rare delayed ocular complication descriptively named frosted branch angiitis.
A Japanese woman in her early fifties was diagnosed with acute-type adult T-cell leukemia-lymphoma associated with human T-cell lymphotropic virus type 1 (HTLV-1). She was managed with whole body irradiation and anti-cancer drugs, followed by allogeneic (donor) human stem cell transplant (HSCT). HSCT allows physicians to use higher doses of chemoradiotherapy as the patient gets an infusion (transplant) of blood-forming stem cells to restore collaterally damaged bone marrow. The patient went into remission and had no complications for several years.
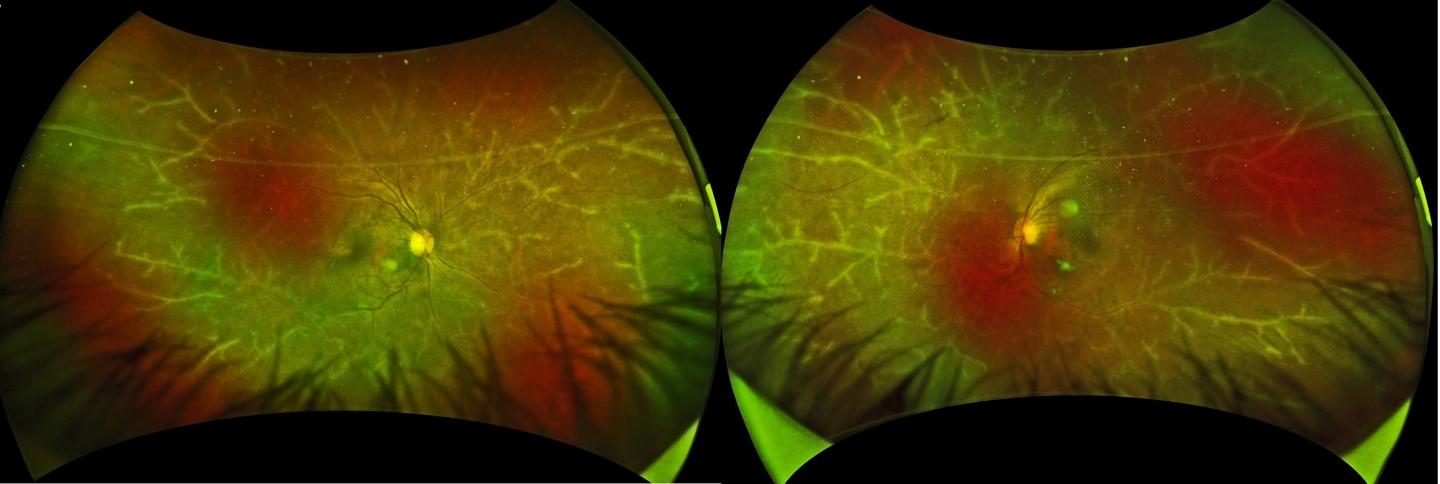
Over four years after HSCT, she developed blurred vision and was referred for further examination. A slit-lamp biomicroscope, which shines a thin sheet of light into the eye for inspection, revealed cellular infiltrates in both segments. Associate Professor Koju Kamoi, lead / corresponding author, describes the remarkably picturesque fundoscopy findings. “Along the retinal blood vessels, a translucent sheath was visible resembling the icy branches of a tree in winter. We recognized this as frosted branch angiitis (Figure A), a rare presentation of florid retinal vasculitis.”
The medical team ran a battery of tests to rule out recurrence, other autoimmune disease, and bacterial, viral or fungal infections. Therefore, the physicians concluded that the frosted branch angiitis resulted from immune activation following HSCT. First described in the Japanese literature by Ito in 1976 occurring in a six-year-old child, frosted branch angiitis is very rare, with most cases reported from Japan and sporadically from other countries.
The patient was treated with corticosteroids to suppress inflammation. After six months the lesion regressed but steroids were continued for over a year. Surprisingly, a month after stopping systemic steroids, the patient developed a skin rash (Figure B) and dryness of both eyes. “This sequence of events suggests that frosted branch angiitis was likely the first sign of systemic inflammation,” explains Dr Kamoi. “Steroids could have suppressed the slower skin and eye-surface changes that were expressed following discontinuation.”
“Though HSCT is beneficial in many situations, it may activate the immune system adversely,” warns Professor Kyoko Ohno-Matsui, senior author. “Frosted branch angiitis could serve as early warning sign of inflammation elsewhere in the body. Therefore, intraocular monitoring is warranted in these patients.”
###
The article, “Frosted branch angiitis after allogeneic haematopoietic stem
cell transplantation in adult T-cell leukaemia-lymphoma” was published in Lancet Haematology. at DOI: 10.1016/S2352-3026(20)30226-X
Media Contact
Koju KAMOI
[email protected]
Original Source
http://www.
Related Journal Article
http://dx.



