NIH grant helps researchers develop new ways to study eye’s repair mechanisms
Credit: The University of Texas at Dallas
Cells called corneal keratocytes are innately programmed to come to the rescue if the eye is injured. This natural healing process sometimes fails, however, resulting in scarring and blindness. Scientists are still trying to understand why.
New research by University of Texas at Dallas bioengineer Dr. David Schmidtke aims to help solve that mystery. Schmidtke and his team have demonstrated a technique in the lab for fabricating tiny strands of collagen called fibrils to facilitate further research on the eye’s repair process. The method was detailed in a new study published in the December issue of the journal Biomedical Microdevices.
The study was funded in part by a $1.8 million, five-year National Institutes of Health grant that Schmidtke received last summer to develop new ways to study the eye’s healing mechanisms — knowledge that may lead to new therapies and treatments.
“How keratocytes repair tissue and why, in some cases, they leave scar tissue, is not well understood,” said Schmidtke, professor of bioengineering in the Erik Jonsson School of Engineering and Computer Science. “We came up with a way to mimic an injury model, so we can look at how the cells respond when there is a wound.”
Dr. Matthew Petroll, professor of ophthalmology and chair of the biomedical engineering graduate program at UT Southwestern Medical Center, initially approached Schmidtke for help in finding a new way to study how the patterning and topography of fibrils can influence corneal cell behavior. These threadlike structures are arranged in a crisscross pattern in the eye and serve as a path to guide keratocytes to an injury.
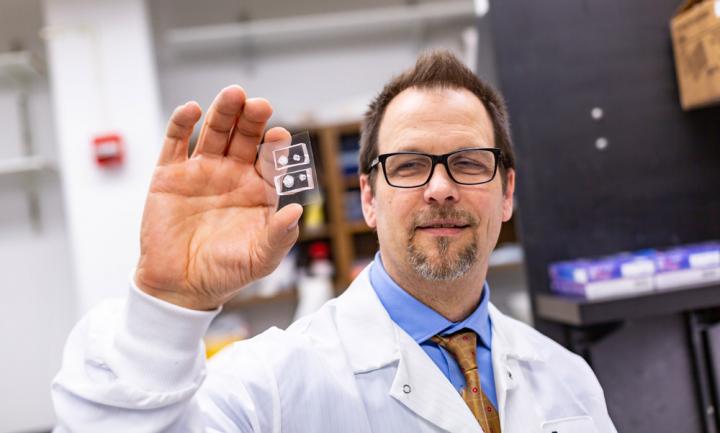
The UT Dallas research draws on Schmidtke’s expertise in microfluidic devices, which are palm-sized pieces of transparent plastic that contain small channels about the size of a strand of human hair. He is using these devices to fabricate the fibrils. Schmidtke’s research team, which includes undergraduate and graduate students, injects collagen into the channels. The collagen polymerizes as it flows through the channels, resulting in aligned fibrils that are similar in structure to the collagen fibrils that are present in corneal tissue.
Schmidtke is working with Dr. Victor Varner, assistant professor of bioengineering at UT Dallas, who is focusing on how keratocytes sense the level of stiffness or softness in the fibrils with which they interact. The researchers plan to study how fibrils’ density, elasticity and dimensionality affect keratocytes. For example, keratocytes behave differently on aligned collagen fibrils compared to randomly oriented collagen fibrils, Schmidtke said.
The research could help develop therapies to reduce corneal scarring and guide efforts to engineer tissue replacements. The models also could be used in other fields where researchers need to study cell patterning and behavior. Schmidtke conducts his research at UT Dallas and in lab space at UT Southwestern.
“The collaboration with UT Southwestern, and having research lab space there, has been a big benefit to applying engineering tools to biomedical questions,” he said.
###
Other authors of the study include Petroll and Varner, UT Dallas biomedical engineering doctoral student Kevin H. Lam, and UT Southwestern doctoral students Pouriska B. Kivanany and Kyle Grose, and postdoctoral research associates Dr. Nihan Yonet-Tanyeri and Dr. Nesreen Alsmadi.
In addition to NIH funding, the research was supported by grants from the Office of the Vice President for Research at UT Dallas, the UT Southwestern Hamon Center for Regenerative Science and Medicine, the UT Southwestern George M. O’Brien Kidney Research Core Center and the nonprofit organization Research to Prevent Blindness.
Media Contact
Media Relations
[email protected]
972-883-2155
Original Source
https:/
Related Journal Article
http://dx.




