Reducing neuroinflammation by disrupting a protein involved in recycling cellular components may provide a potential therapeutic approach for treating neurodegeneration and memory loss.
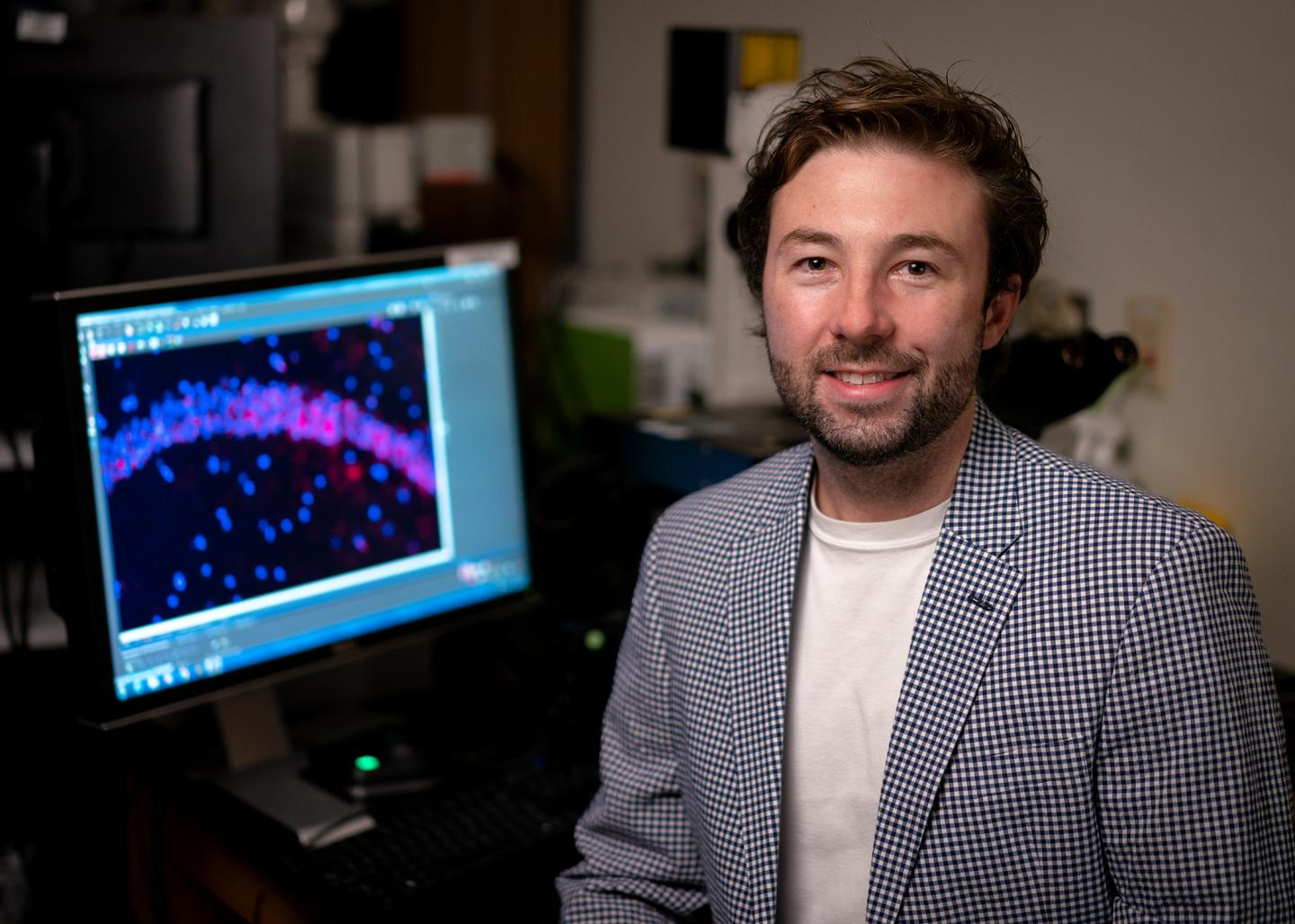
Credit: St. Jude Children’s Research Hospital
Scientists at St. Jude Children’s Research Hospital are advancing understanding of a potential Alzheimer’s disease treatment. The work focuses on LC3-associated endocytosis (LANDO) and its role in neuroinflammation. The results appeared as an advance online publication today in Science Advances.
The researchers previously discovered the LANDO pathway in microglial cells, the primary immune cells of the brain and central nervous system. Scientists found that when genes required for this pathway are deleted, Alzheimer’s disease progression accelerates in a mouse model. The investigators also showed that LANDO protects against neuroinflammation, one of the hallmarks of Alzheimer’s disease.
While continuing to investigate LANDO, the researchers identified a novel function of the protein ATG16L. This protein is critical for autophagy, the normal process by which a cell recycles its components during periods of stress or energy deprivation. While ATG16L is important for autophagy, it can also play a role in LANDO. The investigators found that if a region of ATG16L called the WD domain is deleted, LANDO is inhibited while autophagy continues.
“We learned about this pathway in the context of brain tumor research, but it has major implications for neuroinflammatory and neurodegenerative disease,” said senior author Douglas Green, Ph.D., chair of the St. Jude Immunology Department. “We’ve shown that deficiency in LANDO, combined with aging, can lead to Alzheimer’s disease in a unique mouse model, and there is evidence suggesting that this could also be the case in humans.”
A model for Alzheimer’s disease research
Most mouse models used in Alzheimer’s disease research rely on making genetic changes to recreate the disease. For this work, researchers used a new model with a specific deficiency of just the WD domain of ATG16L. This means the model carries out autophagy normally but lacks the LANDO pathway. By the time the mice are 2 years old, they exhibit symptoms and pathology that mimic human Alzheimer’s disease. This spontaneous age-associated model of Alzheimer’s disease is the first created by deleting a single protein domain (WD on ATG16L), not previously associated with Alzheimer’s disease.
The researchers also analyzed human Alzheimer’s disease tissue samples, looking at the expression of proteins that regulate LANDO, including ATG16L. Expression of these proteins is decreased by more than 50% in people with Alzheimer’s disease. This finding shows a correlation between how deficiency in LANDO combined with aging may lead to Alzheimer’s disease in the mouse model and in humans.
A strategy for treatment emerges
Reducing neuroinflammation has been proposed as a potential way to treat Alzheimer’s disease. To treat their new mouse model, researchers used a compound that inhibits the inflammasome – a complex of proteins that activates pro-inflammatory immune reactions. The scientists targeted the inflammasome responsible for neuroinflammation in people with Alzheimer’s disease. Researchers profiled the model’s behavior and found evidence of improved cognition and memory in addition to a decrease in neuroinflammation.
“This work solidifies LC3-associated endocytosis as a pathway that prevents inflammation and inflammatory cytokine production in the central nervous system,” said first author Bradlee Heckmann, Ph.D., of St. Jude Immunology. “While much of the data on LANDO suggests a significant role in neuroinflammatory and neurodegenerative diseases, there is also a strong possibility that it could be targeted as a therapy against cancer or even infectious diseases that rely on similar processes for survival.”
###
The study’s other authors include Brett Teubner, Emilio Boada-Romero, Bart Tummers, Clifford Guy, Patrick Fitzgerald and Stanislav Zakharenko of St. Jude; and Ulrike Mayer, Simon Carding and Thomas Wileman of the University of East Anglia.
The research was funded in part by grants from the National Institutes of Health (R01AI40646, R35CA231620, F32AI138492, LRPCA231423, R01MH097742 and R01DC012833), the John H. Sununu Endowed Fellowship, an EMBO Long-Term Fellowship, the Biotechnology and Biological Science Research Council, the BBSRC Institute Strategic Programme Gut Microbes and Health, and ALSAC, the fundraising and awareness organization of St. Jude.
St. Jude Children’s Research Hospital
St. Jude Children’s Research Hospital is leading the way the world understands, treats and cures childhood cancer and other life-threatening diseases. It is the only National Cancer Institute-designated Comprehensive Cancer Center devoted solely to children. Treatments developed at St. Jude have helped push the overall childhood cancer survival rate from 20% to 80% since the hospital opened more than 50 years ago. St. Jude freely shares the breakthroughs it makes, and every child saved at St. Jude means doctors and scientists worldwide can use that knowledge to save thousands more children. Families never receive a bill from St. Jude for treatment, travel, housing and food — because all a family should worry about is helping their child live. To learn more, visit stjude.org or follow St. Jude on social media at @stjuderesearch.
Media Contact
Marvin Stockwell
[email protected]
Original Source
http://stjude.
Related Journal Article
http://dx.