SUTD together with the University of Miyazaki developed a novel methodology to provide non-invasive analysis of meniscal implants.
Credit: SUTD
The human knee joint is the largest and complex joint in the body compared to other joints. It has various hard and soft tissue elements to provide stability and proper functioning including the meniscus. The meniscus, a cartilage between the thighbone and the shinbone, acts as a shock absorber to dissipate the body weight and reduce friction during physical activities. Considering, the knee joint is the most used joint in the body, meniscal tears are the most common knee injury due to wear and tear as we age as well as injuries due to sports and trauma.
Meniscal tears can be treated in different ways such as physiotherapy, surgery to remove the torn tissue, replace with allografts, or implants. While meniscal transplants serve as an alternative option, it is technically challenging due to the customization in the sizing required for each person, positioning, securing to the bone, risks of rejection and infection.
Even though a significant amount of work and research has been carried out on prostheses and implants, meniscal implants in particular seem to have been significantly overlooked. It was only in 2015 that the first meniscal got implanted in humans during a clinical trial and more recently in September 2019 that the US’ Food and Drug Administration approved the first artificial meniscus based on clinical trial results.
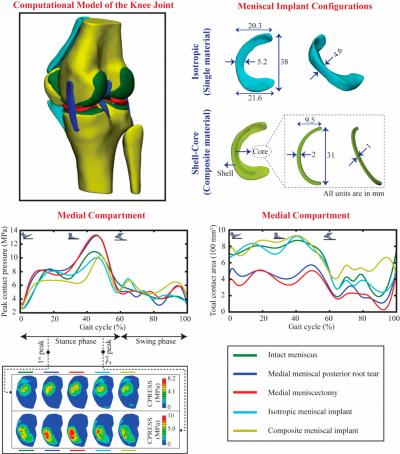
To bridge this research gap, Singapore University of Technology and Design’s (SUTD) Medical Engineering and Design (MED) Laboratory collaborated with the University of Miyazaki’s Biomechanics Laboratory and developed a novel methodology for the early-stage design assessment and verification of meniscal implants using computational modeling and simulation (refer to image). This initial-design stage development paves the way for the manufacturing of 3D printed meniscus, which will allow for customized, anatomically shaped meniscus for a more optimal fit for the patient when they have a meniscal implant. Their research paper has been published in IEEE.
This new development will provide medical practitioners and industry experts valuable insights into understanding how the remnant hard and soft tissues in the knee joint would react biomechanically should an artificial meniscus be implanted. They can then use this information to evaluate aspects of in vivo performance without subjecting patients as well as animals to potential harm or unnecessary risk. Also, the computational models can be used to evaluate options that would otherwise have been impossible experimentally or clinically.
To demonstrate this, the team developed a comprehensive and detailed computational model of an intact knee joint from the medical images and gait cycle data of a healthy adult volunteer. They validated the developed model with biomechanical experiments using the lower extremity of cadavers. They used the validated model to analyze the biomechanical response of soft-tissues in the knee joint for different meniscus conditions, such as intact meniscus, meniscal root tear, total removal of the meniscus, single material meniscal implant and a shell-core composite meniscal implant. Their results suggested that the composite meniscal implant with a shell-core structure performed better than other meniscus conditions and restored the natural biomechanical response of the joint.
This study could also explain the development of knee osteoarthritis due to increased contact stresses and altered joint kinematics caused by the loss of meniscal tissue. This novel synthetic meniscal implantation approach restores the joint mechanics close to the intact meniscus state and appears to be a promising strategy for treating patients with severe meniscal injuries. The model developed in this study sheds light on the knowledge of joint mechanics after injury or repair, and therefore can also assist in the clinical evaluation of other alternative repair techniques.
“This computational model’s ability to study the effects of various meniscal implant configurations in a non-invasive manner provides clinicians and researchers with insights to make more informed decisions and enhance implant designs, positioning, anchoring to the bone as well as the choice of material properties. More importantly, it sets the groundwork for the future of patient-specific 3D printed meniscus for implantation,” said lead researcher, Assistant Professor Subburaj Karupppasamy from SUTD’s Engineering Product Development pillar.
###
Media Contact
Jessica Sasayiah
[email protected]
656-499-4823
Original Source
https:/
Related Journal Article
http://dx.




