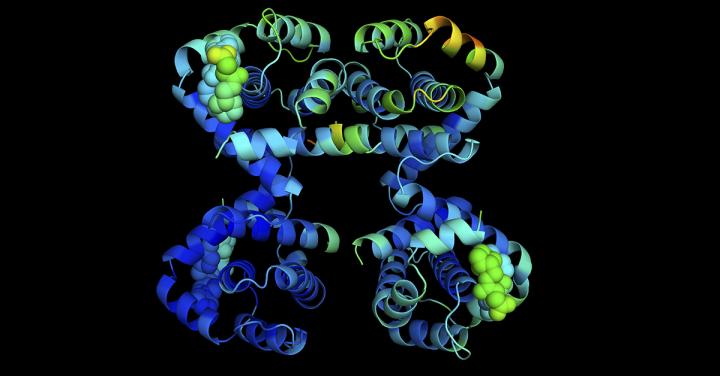
Credit: WEHI, Australia
Australian researchers have identified a protein that could protect the kidneys from ‘bystander’ damage caused by cancer therapies.
The ‘cell survival protein’, called BCL-XL, was required in laboratory models to keep kidney cells alive and functioning during exposure to chemotherapy or radiotherapy. Kidney damage is a common side effect of these widely used cancer therapies, and the discovery has shed light on how this damage occurs at the molecular level.
Inhibiting BCL-XL has been proposed as a potential new cancer therapy, and this research also revealed that in contrast to genetic deletion of BCL-XL, BCL-XL-inhibitory agents can be safely used in laboratory models alone or in combination with other cancer therapies. The research was led by WEHI researchers Dr Kerstin Brinkmann, Dr Stephanie Grabow and Professor Andreas Strasser, and published today in the EMBO Journal.
At a glance
- BCL-XL is a ‘survival’ protein that keeps cells alive and has also been identified as a promising target for anti-cancer agents.
- Our researchers have discovered that BCL-XL protects the kidneys from ‘collateral’ damage during cancer therapy.
- The research also revealed that a research compound that inhibits BCL-XL could be safely used in laboratory models, both alone or in combination with other cancer therapies.
New strategy to investigate BCL-XL
BCL-XL is a widespread ‘survival’ protein, found in many different cell types – but also at high levels in a range of cancers. More than a decade ago, researchers at WEHI and overseas identified BCL-XL as a vital survival factor in oxygen-carrying red blood cells, and platelets, the latter critical for blood clotting. However, the importance of BCL-XL in other cells of adults had not been investigated, said Dr Grabow.
“To address this, we developed a new laboratory model in which the BCL-XL protein was permanently removed from all cells other than blood cells,” Dr Grabow said.
Using this strategy, the team explored whether BCL-XL helped cells to withstand a particularly stressful event – exposure to chemotherapy or radiotherapy, Dr Brinkmann said.
“We discovered that without BCL-XL, kidney cells were highly susceptible to damage by both chemotherapy and radiotherapy. Healthy kidneys remove waste from our body, creating urine, but also maintain healthy numbers of red blood cells by releasing a hormone called erythropoietin (EPO). Without BCL-XL, the kidneys could not perform either of these vital functions,” Dr Brinkmann said.
“Kidney damage is a common side effect of anti-cancer therapies. Our discovery is the first to highlight the role of BCL-XL in protecting kidneys from this damage and may lead to better approaches to reduce this side effect for people undergoing cancer treatment,” she said.
Targeting BCL-XL to treat cancer
Cancer cells are kept alive in our bodies by high levels of survival proteins, such as BCL-XL. New BH3-mimetic drugs that inhibit specific survival proteins have shown great promise in clinical trials. Because BCL-XL is found at high levels in many cancer cells, there has been considerable interest in this protein as a potential target for new anti-cancer agents, Professor Strasser said.
“Unfortunately, early studies showed that administering a BCL-XL inhibitory drug caused a loss of platelets, a serious side effect. To avoid this, the drug could only be administered at levels that, on their own, are not sufficient to efficiently kill cancer cells,” he said.
The team investigated whether short-term inhibition of BCL-XL could be safely combined with other anti-cancer agents – in the hope that inhibition of BCL-XL may make cancer cells more susceptible to chemotherapy or radiotherapy.
“Because we had seen that permanently removing BCL-XL made kidney cells vulnerable to damage, we predicted that this would also occur if BCL-XL were only inhibited for a short period in a laboratory model,” Professor Strasser said.
“We were thrilled to discover that a research compound that inhibits BCL-XL could be administered alone, or at a low dose even in combination with common chemotherapy drugs or radiation therapy without any evidence of kidney damage or other unwanted side effects.
“This suggests a potentially safe way to use candidate drugs that inhibit BCL-XL to treat cancer in clinical trials, even in combination with standard cancer therapies,” Professor Strasser said.
###
The research was supported by the Deutsche Krebshilfe (German Cancer Aid), Leukaemia Foundation Australia, Lady Tata Memorial Trust, University of Melbourne, Cancer Therapeutics CRC, The estate of Anthony (Toni) Redstone OAM, Cure Brain Cancer Australia, Cancer Council of Victoria, Australian Department of Education, Skills and Employment, Leukemia and Lymphoma Society, NHMRC Australia and the Victorian Government.
Media Contact
Vanessa Solomon
[email protected]
Original Source
https:/
Related Journal Article
http://dx.



