Credit: Noam Shemesh, Champalimaud Centre for the Unknown.
Today’s standard procedure to treat rectal cancer includes radical surgery to remove the tumour along with the rectum and its encasing tissue (called mesorectum). After the surgery, the specimen is analysed in the pathology lab to assess, among other things, whether tumour infiltration has occurred into the lymph nodes of the mesorectum. Finally, clinicians consider this and other relevant findings to determine how to proceed with the optimal therapeutic route.
This long-standing approach has been the accepted procedure for rectal cancer treatment for many years. However, it has been reported that radiotherapy and/or chemotherapy can be more effective in high-risk patients (patients with, among other features, lymph node involvement) if administered before the surgery. This observation has placed physicians in a sort of a “Catch 22” situation, where determining the patient’s treatment strategy requires results from the same surgery.
This “Catch 22” can also lead to overtreatment: to be on the safe side, radiologists have traditionally been exceptionally conservative when considering the status of lymph nodes. This cautionary approach works as a double edged sword, since radiation and chemotherapy may have adverse and sometimes irreversible side effects, which clinicians strive to avoid if possible.
Now, in an article published in the scientific journal Cancer Research, a team at the Champalimaud Centre for the Unknown, in Lisbon, Portugal, found a way to help clinicians get out of this “catch”: they developed a cutting-edge, non-invasive, Magnetic Resonance Imaging (MRI) methodology that can efficiently determine whether the tumour has metastasised into the lymph nodes of the mesorectum prior to the surgery.
“The pathologic status of lymph nodes in the mesorectum constitutes one of the most important prognostic markers in rectal cancer patients”, says Inês Santiago, the first author of this study. “However, with currently implemented imaging protocols, knowledge of lymph node status before surgery is limited, so decision-making is largely based on other tumour characteristics.”
To confront this challenge, a multidisciplinary team of scientists and clinicians, including Santiago, a radiologist specialising in rectal cancer, Noam Shemesh, a basic scientist focusing on MRI, and João Santinha, an image analysis expert, decided to develop a novel methodology capable of differentiating between benign and cancerous lymph nodes.
A magnetic signature for cancer
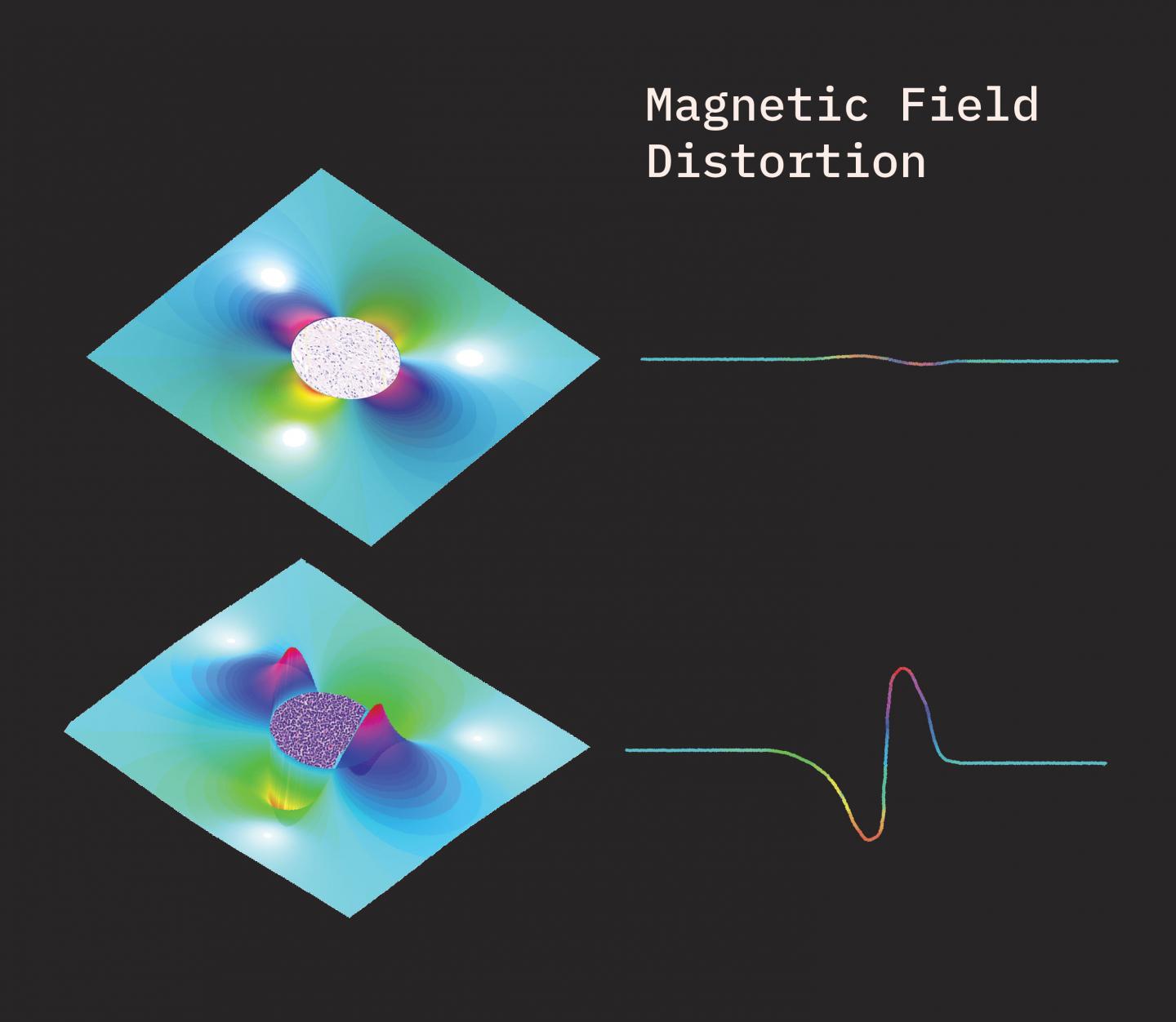
“We know that normal lymph nodes are composed of a relatively uniform distribution of small, loosely-packed cells. By contrast, cancer-involved lymph nodes are characterised by the presence of large, tightly-packed malignant cells”, Shemesh explains. “We knew that this difference in size should induce a kind of “distortion” in local magnetic fields, so we hypothesised that this effect could be exploited to noninvasively differentiate between normal and affected nodes using MRI. To do this, we had to develop a novel MRI methodology, which we named Susceptibility Perturbation Magnetic Resonance Imaging (SPI), as well as a new analysis framework to better understand the sources of its signals.”
The team first tested their hypothesis by harnessing the Centre’s ultra-high magnetic field preclinical MRI scanner – one of the strongest in the world. When samples of lymph nodes excised from rectal cancer patients were imaged with the new SPI methodology, the team immediately observed striking differences between benign and malignant lymph nodes. “Their magnetic signature was quite distinct. And we were also able to confirm our imaging results using the conservative pathological analyses used to assess lymph node malignancy”, Shemesh points out.
After success at this preclinical stage, the team proceeded to adapt SPI for the clinic. “Such ultra-high field scanners are not yet available for human use. Therefore, to make SPI effective for examining lymph node malignancy in patients, we needed to adjust it for conventional scanners, which have a much lower magnetic field”, Santinha explains.
Though it was not clear whether SPI would still work with the lower magnetic fields of clinical scanners, the adaptation was successful. “To confirm the efficacy of SPI, patients were imaged using both SPI and the current ‘gold standard’ MRI method. After surgery, the analysis of the lymph nodes confirmed that SPI increased the accuracy of lymph node characterisation compared with the standard MRI techniques, with a significant improvement in sensitivity and no loss in specificity”, he says.
Now, the team is striving to further optimise clinical SPI and cross-validate the results by extending the study to other centres. “We believe that SPI can be of added value to select patients for pre-operative radiation and chemotherapy. Our results bode well for future studies aiming to generalise SPI as a lymph node specific biomarker, which may be developed to address the lymph node status in other types of cancer as well”, Santiago concludes.
###
Original article: Inês Santiago, João Santinha, Andrada Ianus, Antonio Galzerano, Rita Theias, Joana Maia, Maria João Barata, Nuno Loução, Bruno Costa-Silva, Antonio Beltran, Celso Matos, Noam Shemesh. (2019). Susceptibility perturbation MRI (SPI) maps tumor infiltration into mesorectal lymph nodes. Cancer Research. DOI: 10.1158/0008-5472.CAN-18-3682.
Media Contact
Maria João Soares
[email protected]
Related Journal Article
http://dx.




