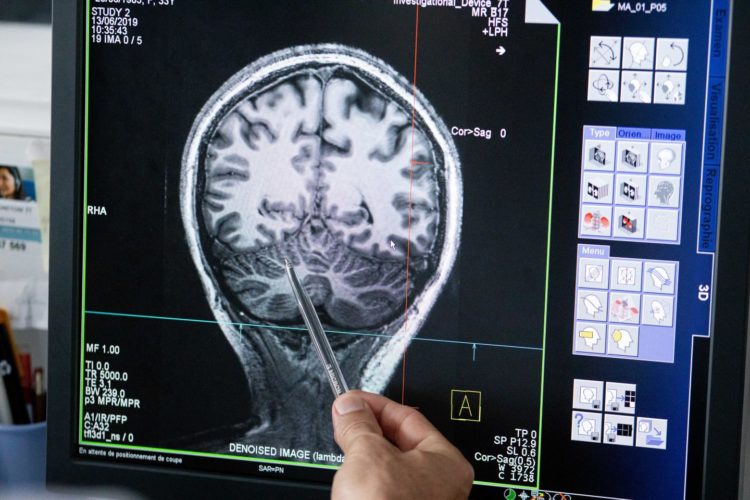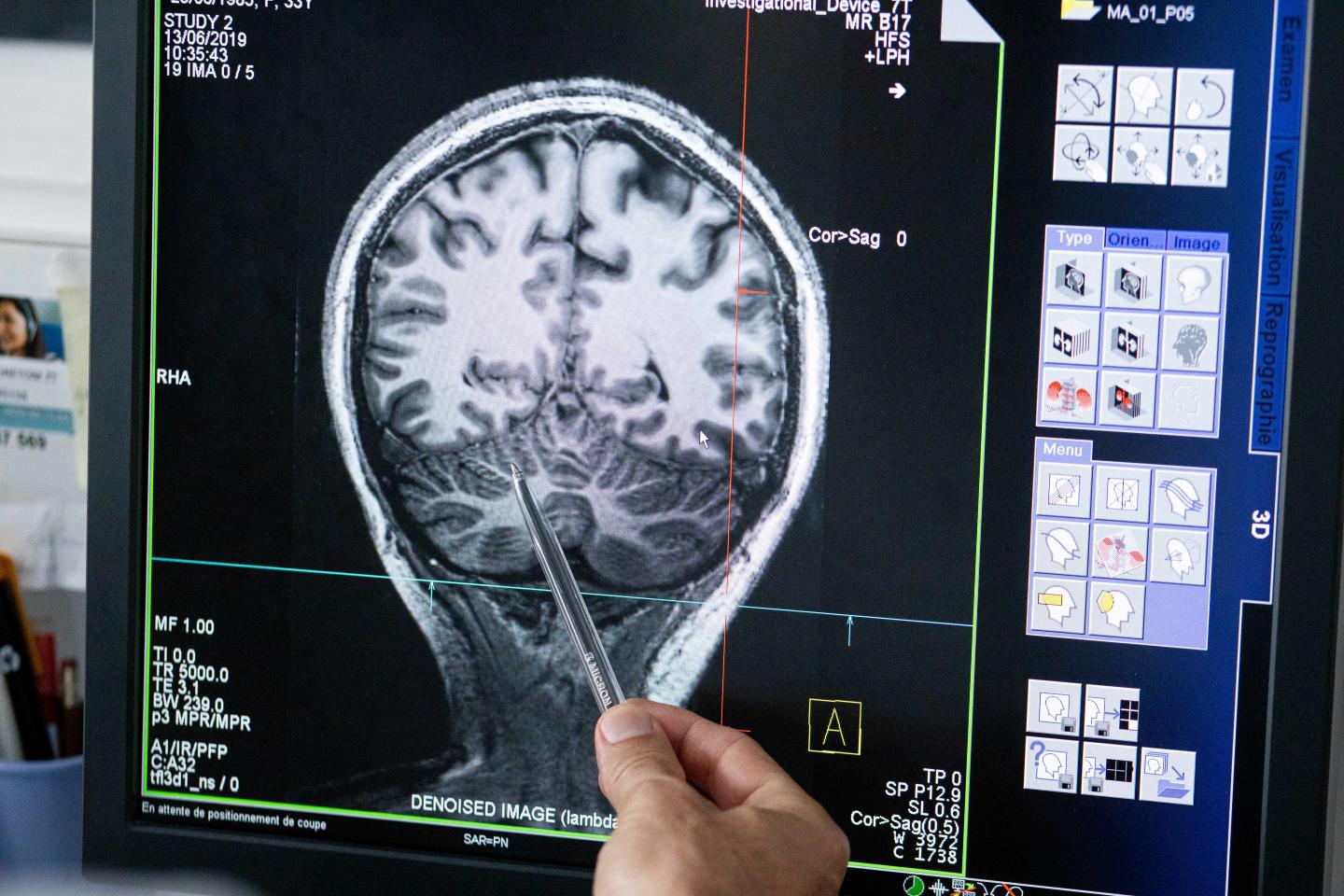
Credit: © INS UMR 1106
In what represents a major milestone on the path to clinical application, a novel method to improve outcomes of Epilepsy surgery has now received approval for clinical testing in 13 French hospitals. The approach could provide a better therapeutic perspective against the drug-resistant form of the disease, which constitutes one third of all cases, and is a development by Human Brain Project scientist Viktor Jirsa and an interdisciplinary team of collaborators. To help clinicians plan surgery strategies, the scientists create personalized brain models of patients and simulate the spread of abnormal activity during epileptic seizures. The method represents the first example of a personalized brain modeling approach entering the clinic and will now be assessed over four years in a cohort of 356 patients under strict requirements.
Epilepsy is a wide-spread neurological disorder that affects around 50 million people worldwide. In many cases, the seizures that mark the disease can be controlled by drugs, but close to a third of all patients are drug resistant. For them, the only remaining option is surgical removal of the epileptogenic zone, the area from which the seizure activity first emerges and then spreads. During surgery preparation it is critical to localize this area as precisely as possible in the brain, but very challenging with current methods. As a result, surgery outcomes are difficult to predict, with success rates of only around 60%.
“This low success rate has largely stayed the same for the last 30 years. We hope our approach can finally improve the odds for patients”, says Prof. Viktor Jirsa. The scientist is Director of Inserm’s Institut de Neurosciences des Systemes (INS) at Aix-Marseille University and Director of Research at CNRS. In the Human Brain Project he is the Deputy Leader of the research area of Theoretical Neuroscience.
Over the last five years and in large part within the framework of the Human Brain Project, Jirsa and his team worked on an approach that could bring a change. The team has adapted the open network simulator The Virtual Brain towards applications in Epilepsy. This work has laid foundations for the project EPINOV, short for “Improving EPilepsy surgery management and progNOsis using Virtual brain technology”, a consortium coordinated by Prof. Fabrice Bartolomei (Hopital de la Timone) that brings together theorists like Jirsa, clinical neuroscientists, in particular from Marseille and Lyon, and the industry partner Dassault Systemes.
After two pilot studies showed promising results for the approach, the EPINOV-consortium has received approval from the French regulatory authority to put their approach to the test in a full-scale multi-centric trial with almost 400 prospective patients.
“It represents the world’s first clinical trial ongoing using full brain network modeling,” says Jirsa. “When the authorization came in, it was like a huge pressure was relieved from me after all this hard work. Then followed last preparations to assure that all steps in the workflow of virtualization and evaluation of the patient brains are in order during the four year period of the trial.”
Fabrice Bartolomei explains “This type of epilepsy affects millions of patients worldwide. The personalized modeling of epilepsy networks in drug-resistant patients is an innovative and scientifically validated approach, which proposes to enrich the interpretation of neurophysiological and neuroimaging tests, and thus to improve the surgical prognosis of epilepsy in an individualized way”.
Viktor Jirsa and his close collaborators Profs. Randy McIntosh at Baycrest Center Toronto and Petra Ritter at Charite Berlin started building The Virtual Brain as an open source brain network simulation engine from 2010 on, using neuronal population models and structural information from neuroimaging.
“In the Human Brain Project environment the conditions were perfect to go the decisive steps further towards applying it in a clinical context. The science underlying this trial is almost entirely a result of our work in the HBP”, the scientist says.
First a personalized brain model is created from data on the individually measured anatomy, structural connectivity and brain dynamics for each patient. Through a series of steps it is turned into a dynamic model, on which the seizure propagation can be simulated. High Performance Computing enables the personalisation of the brain network models through the application of machine learning. The resulting “brain avatar” is customized to the individual patient and allows testing and estimating during surgery preparation. “In a small cohort of retrospective surgery patients we were able to demonstrate that the predictions of the patient’s brain model correlate well with positive surgery outcome”, Jirsa explains, “and other labs have confirmed our results independently.”
In half of the cases, the surgeons will have information from the Epilepsy-model in their staff meetings, where therapeutic interventions are planned. “It´s a blind random design, half of these patients will be operated taking our model predictions into account, the other half will not. After four years, the statistics will show us hopefully to what degree the model predictions changed the surgery practice, results, and outcome”, Jirsa says.
Within the Epinov consortium the industrial partner Dassault Systemes will develop a virtual brain-based simulation software prototype that could subsequently be provided to clinics worldwide. Headquartered in France, Dassault Systemes is a multinational software company focused on 11 industries including life sciences and the development of patient-centric modeling and simulation experiences.
“There is a very big responsibility”, Jirsa emphasizes “and at the same time it’s very exciting that we have this chance to improve clinical practice and ultimately patients’ lives. And if the approach succeeds, it would also be the first modelling-based example of personalized medicine that makes the jump from research to clinical practice – so the outcome will certainly be a signal to the field”.
Prof. Katrin Amunts, Scientific Research Director of the Human Brain Project, highlights the significance of the move into the clinic: “This breakthrough by Viktor Jirsa and his colleagues is a fantastic example of a new type of technology-enabled computational neuro-medicine. It is one of our central aims to catalyze developments like this that make concrete contributions in the fight against brain diseases to benefit patients.”
Prof. Philippe Ryvlin, who leads the Medical Informatics Platform in HBP and the epilepsy surgery section of the European Reference Network EpiCARE emphasises that “this clinical trial, which will be the largest randomised study ever performed in epilepsy surgery, demonstrates that simulation of the human brain, as developed in HBP, has now reached a stage where it can be readily applied to address unmet medical needs.”
Virtual Brain Researchers are also continuing their activities on clinical modeling for stroke and Alzheimer’s in collaboration with experts that the HBP brings together. For Jirsa seeing his work as a theoretical scientist gain this potential impact has been the result of a unique convergence: “That we have come to this point was made possible by clinical expertise and our activities on The Virtual Brain and the Human Brain Project all coming together – right place, right time, right people.”
###
Media Contact
Peter Zekert
[email protected]
49-024-616-196-860
Original Source
https:/