In a groundbreaking development that could revolutionize the treatment landscape for prostate cancer, recent research has illuminated the complex interplay between gut microbiota—specifically the bacterial genus Ruminococcus—and prostate tumor biology. This new insight into the gut–prostate axis not only deepens our understanding of the microbiome’s systemic influence but also unveils promising therapeutic avenues previously unconsidered in oncology. The study, led by Liu, Wang, Wu, and colleagues, offers a compelling narrative on how these gut microbes may modulate cancer progression, opening up potential for microbiota-targeted interventions in managing prostate cancer.
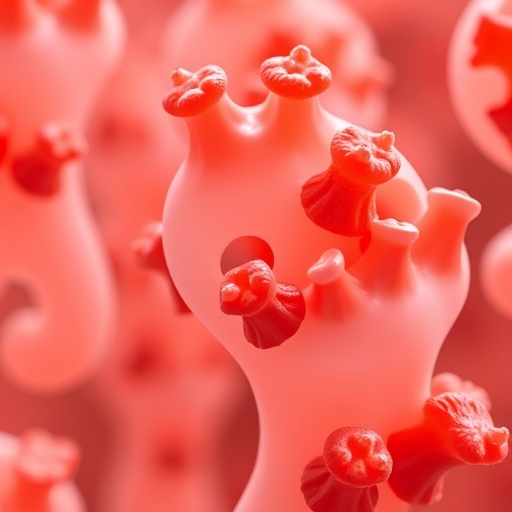
The central tenet of this research hinges on the recognition that the gut microbiome does far more than aid digestion; it orchestrates a symphony of metabolic and immunological signals that ripple throughout the body. Among the myriad microbial players, Ruminococcus has emerged as a particularly influential genus. Known for its role in fermenting complex carbohydrates and producing short-chain fatty acids (SCFAs), Ruminococcus influences systemic inflammation and metabolic homeostasis—processes intimately linked to cancer pathophysiology. The study posits that alterations in Ruminococcus populations could directly impact prostate tumor microenvironments, potentially accelerating or mitigating tumorigenesis.
A defining feature of prostate cancer is its heterogeneity and variable response to existing therapies. Current treatment modalities, including surgery, radiation, androgen deprivation therapy, and chemotherapy, often face limitations such as adverse side effects and eventual resistance. This has propelled scientists to seek novel, more holistic targets. By dissecting the gut–prostate axis, researchers are exploring whether the manipulation of gut microbiota might sensitize tumors to conventional treatments or even suppress malignant phenotypes independently. The implications could be profound, shifting paradigms toward microbiome-informed precision medicine.
.adsslot_DYN1MRe7jZ{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_DYN1MRe7jZ{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_DYN1MRe7jZ{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Technically, the researchers employed advanced metagenomic sequencing and metabolomic profiling to map the gut microbial community structure and metabolite signatures in prostate cancer patients versus healthy controls. Strikingly, Ruminococcus abundance was significantly altered in cancer patients, correlating with distinct metabolic fingerprints suggestive of inflammatory and oncogenic signaling. The study further analyzed host immune parameters, revealing that microbial dysbiosis affects systemic immune modulators such as cytokines and T-cell activation states—key determinants in cancer immunosurveillance and progression.
These findings align with a burgeoning body of literature implicating the microbiome in cancer initiation and progression, but Liu et al. push the envelope by pinpointing a specialized bacterial genus within a discrete organ axis. The gut–prostate relationship is particularly intriguing given the prostate’s proximity to the lower gastrointestinal tract and its susceptibility to systemic metabolic and immune influences derived from microbial metabolites. This pioneering focus on Ruminococcus redefines our spatial and functional understanding of microbiota-cancer interactions.
Immunologically, the study identifies a link between Ruminococcus abundance and the regulation of T-regulatory cells (Tregs) and cytotoxic CD8+ T lymphocytes within the tumor milieu. Elevated Ruminococcus levels correlated with immunosuppressive environments favoring tumor immune evasion, whereas diminished populations appeared to restore effective antitumor immunity. This suggests that modulating Ruminococcus could tip the immune balance toward tumor eradication, complementing existing immunotherapies which have so far shown limited success in prostate cancer.
The translational potential is vast. One envisaged approach involves probiotics or dietary interventions designed to recalibrate Ruminococcus populations, thereby reshaping metabolic and immune landscapes to restrain tumor growth. Alternatively, targeted antibiotics or phage therapies could selectively disrupt pathogenic strains without compromising overall microbiome integrity. Integrating microbiota modulation with androgen deprivation or checkpoint blockade therapy could enhance efficacy and overcome resistance mechanisms.
Nevertheless, the researchers caution that the gut microbiome’s complexity necessitates a nuanced understanding to avoid unintended consequences. Dysbiosis induced by broad-spectrum interventions might perturb beneficial microbial networks, underscoring the need for precision microbiome editing technologies. Importantly, interindividual variability in microbiota composition means therapies must be personalized, supported by robust biomarker platforms capable of real-time microbial monitoring.
In anticipation of clinical translation, the team advocates for longitudinal studies tracking microbiome dynamics through prostate cancer progression and treatment courses. Such data can elucidate causal relationships and temporal windows where microbiome-targeted therapies may be most effective. Furthermore, integrating metagenomic data with host genomics and immune profiling could refine patient stratification, enabling bespoke therapeutic regimens that factor in the gut–prostate axis status.
The research has sparked excitement beyond the oncology community by challenging traditional views that confine cancer etiology to genetic mutations and local tumor microenvironment. Instead, it propels the narrative that cancer is a systemic disease intertwined with microbial ecosystems. This paradigm shift invites cross-disciplinary collaborations spanning microbiology, immunology, oncology, and computational biology to harness microbiota’s full therapeutic potential.
Experts in the field have praised the study for opening a novel frontier in prostate cancer research. “This work elegantly illustrates how a single microbial genus can have ripple effects on tumor biology,” said Dr. Andrea Chen, a senior oncologist not affiliated with the study. “It sets a foundation for innovative treatments that complement and possibly surpass current modalities by leveraging our microbiome’s influence.”
While human clinical trials are yet to commence, preclinical models incorporating microbiota manipulation have demonstrated promising antitumor effects, reinforcing the translational promise of these findings. The challenge now lies in fine-tuning intervention strategies to achieve durable, reproducible outcomes in diverse patient populations.
In conclusion, the elucidation of Ruminococcus’s involvement in the gut–prostate axis represents a milestone in cancer biology, offering a fresh perspective on disease modulation through microbial ecosystems. This intersection of microbiology and oncology paves the way for transformative therapeutic strategies that may ultimately reduce prostate cancer’s global burden. As research progresses, the hope is to transform the gut microbiome from a mysterious black box into a wellspring of oncological innovation with tangible benefits for patients worldwide.
Subject of Research: The role of Ruminococcus in the gut–prostate axis and its impact on prostate cancer progression and treatment opportunities.
Article Title: Ruminococcus and prostate cancer: new treatment opportunities on the gut–prostate axis.
Article References:
Liu, Y., Wang, Y., Wu, G. et al. Ruminococcus and prostate cancer: new treatment opportunities on the gut–prostate axis. Med Oncol 42, 387 (2025). https://doi.org/10.1007/s12032-025-02951-7
Image Credits: AI Generated
Tags: gut microbiota and prostate cancergut-prostate cancer axismetabolic homeostasis and cancermicrobial modulation of tumor progressionmicrobiome’s influence on cancermicrobiota-targeted interventionsprostate cancer treatment innovationsRuminococcus and tumor biologyshort-chain fatty acids and healthsystemic inflammation and cancertherapeutic avenues in oncologyunderstanding cancer heterogeneity