Glioblastoma stands as one of the most devastating and treatment-resistant forms of brain cancer, characterized by rapid proliferation and aggressive invasion into surrounding brain tissue. Current treatment protocols, which typically combine maximal surgical resection, radiation therapy, and chemotherapy using temozolomide, unfortunately yield dismal survival outcomes, with most patients living only 12 to 18 months post-diagnosis. This grim prognosis underscores an urgent need for more effective therapeutic interventions that not only target tumors with higher precision but also overcome the biological barriers unique to the central nervous system.
At the forefront of addressing this challenge is Michael Gomes, a PhD candidate at the Wits Advanced Drug Delivery Platform (WADDP), who has recently been awarded the prestigious 2026 South African Medical Research Council (SAMRC) Institutional Clinician Researcher Development Programme scholarship. This grant empowers Gomes to accelerate his innovative research focused on developing nanoparticle-based drug delivery systems engineered specifically for glioblastoma treatment. His interdisciplinary work intertwines clinical insights with nanotechnology, aiming to revolutionize how chemotherapy agents reach and eradicate brain tumors.
One of the pivotal obstacles in glioblastoma therapy is the blood-brain barrier (BBB), a physiological safeguard that limits the penetration of many systemic chemotherapy agents into the brain. This barrier, while protecting neural tissue from toxins and pathogens, also inadvertently restricts drug delivery to tumor sites, rendering many conventional treatments ineffective. Addressing this, Gomes’s research explores advanced nanoscale drug carriers capable of surmounting the BBB or bypassing it altogether, ensuring a sufficient concentration of chemotherapeutic drugs directly at the tumor microenvironment.
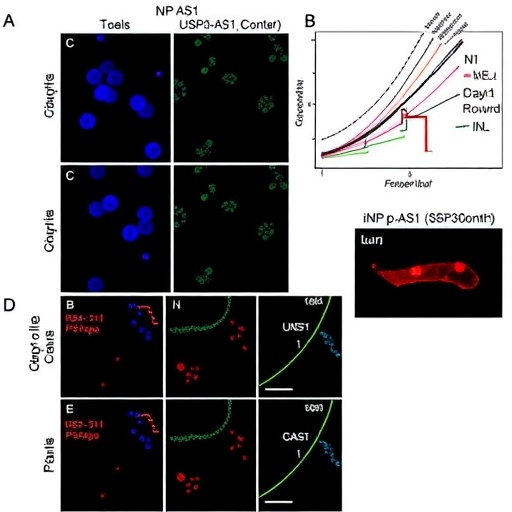
The project systematically evaluates three distinct nanoparticle platforms: liposomes, polymer-based particles, and polydopamine nanoparticles. Liposomes—lipid bilayer vesicles—are renowned for their biocompatibility and have already been employed successfully in various drug delivery contexts due to their ability to encapsulate hydrophilic and hydrophobic compounds alike. Polymer-based nanoparticles, often synthesized from biodegradable polymers such as poly(lactic-co-glycolic acid) (PLGA), offer controlled release profiles and can be functionally tailored to respond to the tumor’s biological milieu, such as pH or enzymatic activity.
The most novel aspect of Gomes’s investigation focuses on polydopamine nanoparticles. Inspired by dopamine, a neurotransmitter intrinsically present in the brain, polydopamine exhibits remarkable adhesive properties, photo- and chemo-stability, and exceptional biocompatibility. This synthetic polymer holds promise as a versatile drug carrier platform, potentially achieving enhanced cellular uptake and targeted delivery. Its inherent similarity to endogenous brain molecules may facilitate safer interactions and reduce immune responses, a critical consideration in neuro-oncological therapeutics.
Furthermore, Gomes’s research ventures beyond traditional drug administration routes by leveraging the glymphatic system—a recently elucidated cerebrospinal fluid (CSF)-mediated waste clearance pathway in the brain. Unlike systemic delivery, which requires crossing the BBB, the glymphatic route allows agents introduced directly into the CSF to diffuse through perivascular spaces and navigate towards brain tissues, including tumor sites. This paradigm shift in drug delivery could heighten tumor-targeted drug concentrations while minimizing systemic toxicity, representing a transformative approach in glioblastoma therapy.
This pioneering work exemplifies the power of integrating cutting-edge nanotechnology with an in-depth understanding of neurophysiology. By exploiting the glymphatic system, Gomes aims to surmount the inherent obstacles imposed by the BBB, tailoring drug delivery systems that mirror the brain’s natural transport mechanisms. Achieving effective chemotherapy delivery via this pathway could redefine therapeutic strategies, potentially improving survival and quality of life for glioblastoma patients globally.
Supported by the SAMRC Clinician Researcher Development Programme, the scholarship reflects a strategic investment in cultivating clinician-scientists who bridge the gap between bench and bedside. Gomes’s dual training as a medical student and researcher positions him uniquely to identify unmet clinical needs and translate laboratory discoveries into tangible therapeutic innovations. His ultimate ambition is to specialize in neurosurgery, integrating surgical expertise with research insights to develop and refine treatment modalities for brain cancer.
Under the mentorship of distinguished experts including Dr. Divesha Essa, Dr. Nnamdi Ikemefuna Okafor, Professor Dinesh Naidoo, and Professor Yahya Choonara at WADDP, Gomes’s research benefits from an environment dedicated to translational science. Essa emphasizes the indispensable role of clinician-scientists in ensuring that scientific breakthroughs pragmatically address patient care complexities. “Their clinical exposure equips them with nuanced understanding that informs the design and implementation of more effective therapies,” she notes.
The collaborative ecosystem at WADDP, combining state-of-the-art laboratory modeling, neurosurgical expertise, and advanced drug delivery platforms, epitomizes a modern approach to tackling brain tumors. This confluence permits realistic in vitro and in vivo evaluations of novel drug carriers, optimizing formulations in the context of clinical realities. As Choonara articulates, fostering early-career investigators through such scholarships is vital for sustaining innovation pipelines capable of delivering relevant, patient-centered solutions.
In essence, Michael Gomes’s research represents a beacon of hope amidst the daunting challenge posed by glioblastoma. By integrating innovative nanoparticle systems, exploiting the glymphatic pathway, and maintaining a keen focus on clinical translatability, his work aspires to elevate brain cancer therapeutics beyond current limitations. The ultimate goal is not only to prolong survival but also to enhance the quality of life for patients confronting this aggressive disease.
His pursuit underscores the critical importance of merging scientific ingenuity with clinical acumen, a synergy that promises to unlock new horizons in the fight against one of the most formidable cancers. As this research evolves, it may lay the groundwork for groundbreaking therapies capable of overcoming the biological and technical barriers that have long hindered progress in neuro-oncology.
Subject of Research: Nanoparticle-based drug delivery systems for glioblastoma, emphasizing polydopamine nanoparticles and the glymphatic system.
Article Title: Cutting-Edge Nanoparticle Therapeutics Illuminate New Pathways Against Glioblastoma
News Publication Date: Not specified (2026 implied)
Web References:
Wits Advanced Drug Delivery Platform (WADDP) — https://www.wits.ac.za/waddp/
Academic profiles of supervising researchers linked via Wits University
Image Credits: WADDP
Keywords: Brain cancer, Glioblastoma, Nanoparticles, Polydopamine, Drug delivery, Blood-brain barrier, Glymphatic system, Neurosurgery, Chemotherapy
Tags: advanced nanotechnology in oncologybrain cancer precision medicine advancementsglioblastoma treatment innovationsimproving survival rates in glioblastomainterdisciplinary approaches in cancer therapyMichael Gomes glioblastoma researchnanoparticle drug delivery for brain cancerovercoming blood-brain barrier in chemotherapySouth African Medical Research Council scholarship recipientstargeted therapy for brain tumorstemozolomide limitations in brain cancerWits Advanced Drug Delivery Platform research