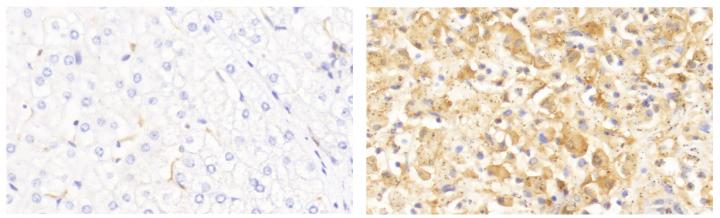
Credit: Belkaya et al., 2019
Researchers have identified a genetic mutation that caused an 11-year-old girl to suffer a fatal reaction to infection with the Hepatitis A virus (HAV). The study, which will be published June 18 in the Journal of Experimental Medicine, reveals that mutations in the IL18BP gene causes the body’s immune system to attack and kill healthy liver cells, and suggests that targeting this pathway could prevent the deaths of patients suffering rapid liver failure in response to viral infection.
HAV infects the liver and usually causes a relatively mild illness that clears up in a matter of weeks or months. But as many as 1 in 200 HAV patients suffer a much more severe response known as fulminant viral hepatitis (FVH) that is characterized by a rapid loss of liver tissue and catastrophic liver failure, resulting in the release of toxins that damage the brain. The condition is usually fatal unless the patient receives a liver transplant.
Other hepatitis viruses can also cause FVH, but the reason why some patients suffer such a severe response to infection is unclear. It typically occurs in children and young adults who are otherwise healthy and have no prior history of liver disease or immunodeficiencies.
A team of researchers led by Professor Jean-Laurent Casanova at The Rockefeller University in New York identified an 11-year-old girl in France who died of FVH after becoming infected with HAV. The researchers sequenced the girl’s DNA and discovered that she carried identical mutations in both copies of the IL18BP gene, which encodes a protein called interleukin-18 binding protein (IL-18BP).
IL-18BP can bind and neutralize interleukin-18 (IL-18), a powerful ‘cytokine’ molecule that the body produces in response to infection in order to activate certain types of immune cells and promote inflammation. Casanova and colleagues determined that the mutation identified in the patient’s IL18BP gene prevented the IL-18BP protein from neutralizing IL-18.
To understand how this might affect the body’s response to HAV infection, the researchers incubated human liver cells with Natural Killer (NK) cells, a type of immune cell that targets virally infected cells. Casanova and colleagues discovered that, in the absence of IL-18BP, IL-18 enhanced NK cells’ ability to target and kill liver cells, whether they were infected with HAV or not. Addition of IL-18BP blocked this IL-18-induced toxicity, suggesting that IL-18BP usually prevents an excessive reaction to HAV infection but that patients carrying mutations in this gene are susceptible to FVH.
“Our findings provide a proof of principle that FVH can be caused by inborn errors in single genes,” Casanova says. “Human IL-18BP injections have been approved for clinical use for indications unrelated to liver conditions and has been proposed as a treatment for preventing acetaminophen-induced liver damage. Neutralizing IL-18 with IL-18BP might be beneficial to patients with FVH caused by HAV and possibly other viruses as well.”
###
Belkaya et al. 2019. J. Exp. Med. http://jem.
About the Journal of Experimental Medicine The Journal of Experimental Medicine (JEM) features peer-reviewed research on immunology, cancer biology, stem cell biology, microbial pathogenesis, vascular biology, and neurobiology. All editorial decisions are made by research-active scientists in conjunction with in-house scientific editors. JEM makes all of its content free online no later than six months after publication. Established in 1896, JEM is published by Rockefeller University Press. For more information, visit jem.org.
Visit our Newsroom, and sign up for a weekly preview of articles to be published. Embargoed media alerts are for journalists only.
Follow JEM on Twitter at @JExpMed and @RockUPress.
Media Contact
Ben Short
[email protected]
Related Journal Article
http://dx.




