Medical University of South Carolina researchers report that adding a compound to reduce inflammation to standard stroke treatment improves learning, memory and motor recovery and may extend the treatment window by reducing risk of hemorrhage
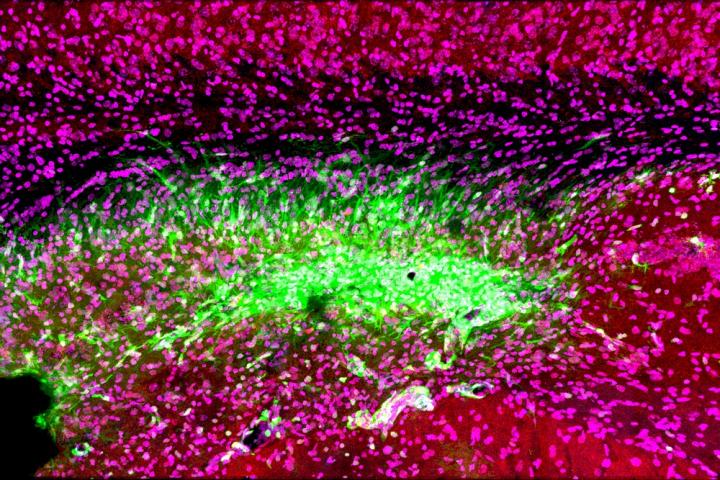
Credit: Medical University of South Carolina. Image courtesy of Dr. Stephen Tomlinson.
Reperfusion therapy, the gold standard for stroke treatment, helps restore blood flow after a stroke caused by a clot, preventing loss of brain tissue. However, only about 10% of stroke patients qualify, in part because of reperfusion therapy’s narrow treatment window.
A recent Medical University of South Carolina study suggests that this therapy could be both safer and more effective for both motor and cognitive recovery if administered with a specialized compound that blocks the immune response. The team’s preclinical findings, reported in the cover article of the May 13 Journal of Neuroscience, suggest that reducing the immune response in the brain could be a strategy for improving cognitive recovery. It could also extend the treatment window for therapy, allowing stroke specialists to help many more stroke patients.
“With reperfusion therapy, we’re restoring the blood flow, which is necessary to save the tissue, but there is an ongoing inflammatory response by the immune system that is not targeted by reperfusion,” said Stephen Tomlinson, Ph.D., interim chair of the Department of Microbiology and Immunology at MUSC and senior author of the article.
This could explain why, though mechanical reperfusion has a success rate of 90% in returning blood flow to the brain, only about 40% of treated patients recover enough motor and reasoning skills within three months to tend to their daily needs independently. Even those who do recover motor function can still struggle with cognitive challenges months later.
“I’ve seen patients who have barely any motor deficits at follow-up, but they’re really struggling in their daily life in terms of memory, behavioral consequences and language,” said lead author Ali Alawieh, M.D., Ph.D., who completed his graduate studies at MUSC and is now a resident in neurosurgery at Emory University School of Medicine.
Tomlinson and Alawieh think the immune response in the brain is the culprit.
During a stroke, the oxygen and energy supply to the brain is cut off by a clot, causing brain tissue to become stressed and die rapidly.
Just as it is with a cut to the knee, the immune system is activated to heal the wound, which includes clearing the dead tissue.
A family of special immune proteins called complement proteins help to guide and promote this immune response in the damaged areas.
In a 2018 article in Science Translational Medicine, Tomlinson and Alawieh showed that these complement proteins flagged both dead tissue and stressed brain cells for removal.
The stressed brain cells were not yet dead, only damaged by lack of oxygen and energy. As the goal of stroke treatment is to save as much brain tissue as possible to lessen overall damage, this was a concerning result, as it meant salvageable tissue was being destroyed by the immune system.
Therefore, Tomlinson and his team developed a complement protein blocker, named B4Crry, which acts only at the site of stroke injury. This compound blinds the complement proteins to the signals of stressed brain cells, saving the stressed tissue and reducing overall brain damage in a preclinical stroke model.
In the current study, Tomlinson and Alawieh hypothesized that pairing reperfusion therapy and B4Crry would significantly improve stroke recovery beyond reperfusion therapy alone. In particular, they hypothesized this combination treatment would improve cognitive recovery.
As Tomlinson’s team expected, reperfusion therapy alone did improve recovery of coordinated movements such as walking in a preclinical model of stroke. With the addition of B4Crry to treatment, coordinated movement improved even faster, with greater recovery seen as early as three days after the stroke.
The improvements to learning and memory were even greater than those seen with motor functions.
Reperfusion therapy alone was equal to no treatment at all for learning and memory recovery after stroke. However, when B4Crry was added to their treatments, mice had greatly improved cognitive recovery, making three times fewer errors on a learning and memory task.
Tomlinson’s team further probed into why the addition of B4Crry, and the subsequent reduction of the brain’s immune response, aided cognitive recovery so greatly.
They found that after stroke, brain immune cells called microglia began eating the connections between stressed brain cells. Immune system complement proteins were marking these connections for destruction because they displayed the stressed cell signal. Without these connections, brain cells cannot communicate efficiently, and overall brain function decreases.
B4Crry concealed the cells’ stress signals from the complement proteins and thereby saved the connections between neurons. Preserving connectivity improved learning and memory brain function after stroke.
A complement inhibitor such as B4Crry might also help stroke specialists overcome the biggest hurdle for reperfusion therapy: the short treatment window.
Tomlinson’s team showed that after clot removal adding B4Crry to reperfusion therapy reduced the potential for hemorrhage, or excessive bleeding, even with treatment given up to six hours after the stroke. These findings suggest that complement inhibition could not only make reperfusion therapy safer but extend its treatment window, making it available for many more stroke patients.
Alawieh is excited about the future use of complement inhibition in the clinic.
“Our next step is to see how complement inhibitors work with comorbidities, such as old age, smoking and diabetes, in a preclinical study,” he explained. “Collectively, this information will help us design the best clinical trial when we move to humans.”
Tomlinson’s team at MUSC is also testing the potential for complement inhibitors in other brain injuries, such as traumatic brain injury.
“We have shown that we can administer complement inhibitors as far as two months after a traumatic brain injury and see improvements in cognitive recovery,” said Tomlinson. “This is something I’m actually quite excited about. It means that months after an initial event, complement inhibitors could still be beneficial to cognitive recovery after brain injuries, including strokes.”
###
Disclosure: Dr. Stephen Tomlinson is an inventor on a patent application for natural antibody-targeted complement inhibitors filed by the University of Colorado (PCT/US2014/012831; targeting constructs based on natural antibodies and uses thereof) and is a consultant for Admirx Inc., a company developing complement inhibitors.
About the Medical University of South Carolina
Founded in 1824 in Charleston, MUSC is the oldest medical school in the South as well as the state’s only integrated academic health sciences center with a unique charge to serve the state through education, research and patient care. Each year, MUSC educates and trains more than 3,000 students and 800 residents in six colleges: Dental Medicine, Graduate Studies, Health Professions, Medicine, Nursing and Pharmacy. The state’s leader in obtaining biomedical research funds, in fiscal year 2019, MUSC set a new high, bringing in more than $284 million. For information on academic programs, visit http://musc.
As the clinical health system of the Medical University of South Carolina, MUSC Health is dedicated to delivering the highest quality patient care available while training generations of competent, compassionate health care providers to serve the people of South Carolina and beyond. Comprising some 1,600 beds, more than 100 outreach sites, the MUSC College of Medicine, the physicians’ practice plan and nearly 275 telehealth locations, MUSC Health owns and operates eight hospitals situated in Charleston, Chester, Florence, Lancaster and Marion counties. In 2019, for the fifth consecutive year, U.S. News & World Report named MUSC Health the No. 1 hospital in South Carolina. To learn more about clinical patient services, visit http://muschealth.
MUSC and its affiliates have collective annual budgets of $3.2 billion. The more than 17,000 MUSC team members include world-class faculty, physicians, specialty providers and scientists who deliver groundbreaking education, research, technology and patient care.
Media Contact
Heather Woolwine
[email protected]
Related Journal Article
http://dx.




