By identifying one of the mechanisms regulating the virulence of Pseudomonas aeruginosa, a UNIGE team is proposing a new strategy to combat this bacterium, which is resistant to many common antibiotics
Pseudomonas aeruginosa is an opportunistic pathogenic bacterium present in many ecological niches, such as plant roots, stagnant water or even the pipes of our homes. Naturally very versatile, it can cause acute and chronic infections that are potentially fatal for people with weakened immune systems. The presence of P. aeruginosa in clinical settings, where it can colonise respirators and catheters, is a serious threat. In addition, its adaptability and resistance to many antibiotics make infections by P. aeruginosa increasingly difficult to treat. There is therefore an urgent need to develop new antibacterials. Scientists from the University of Geneva (UNIGE), Switzerland, have identified a previously unknown regulator of gene expression in this bacterium, the absence of which significantly reduces the infectious power of P. aeruginosa and its dangerous nature. These results, to be published in the journal Nucleic Acid Research, could constitute an innovative target in the fight against this pathogen.
RNA helicases perform essential regulatory functions by binding and unwinding various RNA molecules to perform their functions. RNA helicases are present in the genomes of almost all known living organisms, including bacteria, yeast, plants, and humans; however, they have acquired specific properties depending on the organism in which they are found. “Pseudomonas aeruginosa has an RNA helicase whose function was unknown, but which was found in other pathogens”, explains Martina Valentini, a researcher leading this research in the Department of Microbiology and Molecular Medicine at UNIGE Faculty of Medicine, and holder of an SNSF “Ambizione» grant. “We wanted to understand what its role was, in particular in relation to the pathogenesis of the bacteria and their environmental adaptation.”
A severely reduced virulence
To do this, the Geneva team combined biochemical and molecular genetic approaches to determine the function of this protein. “In the absence of this RNA helicase, P. aeruginosa multiplies normally in vitro, both in a liquid medium and on a semi-solid medium at 37°C”, reports Stéphane Hausmann, a researcher associate in the Department of Microbiology and Molecular Medicine at UNIGE Faculty of Medicine and first author of this study. “To determine whether the infection capacity of the bacteria was affected, we had to observe it in vivo in a living organism.”
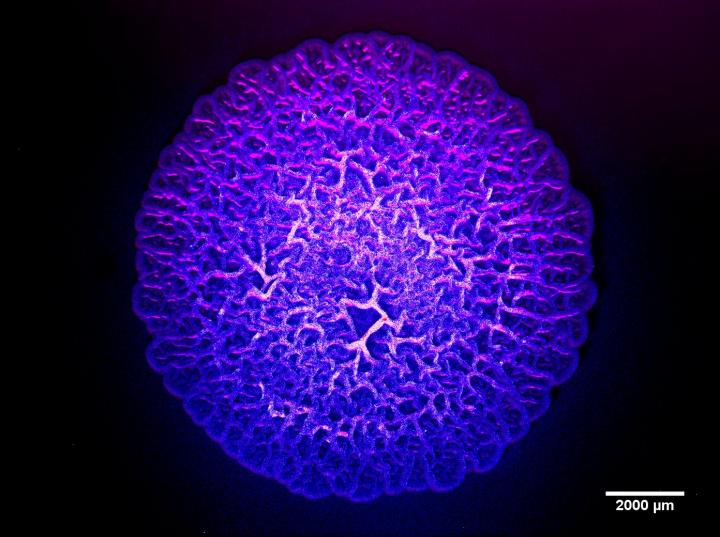
The scientists then continued their research using Galleria mellonella larvae, a model insect for studying host-pathogen interactions. Indeed, the innate immune system of insects has important similarities with that of mammals. Moreover, these larvae can live at temperatures between 5°C and 45°C, which makes it possible to study bacterial growth at different temperatures, including that of the human body. Three groups of larvae were observed; the first, after injection of a saline solution, saw 100% of its population survive. In the presence of a normal strain of P. aeruginosa, less than 20% survived at 20 hours after infection. In contrast, when P. aeruginosa no longer possessed the RNA helicase gene, over 90% of the larvae remained alive. “The modified bacteria became almost harmless, while remaining very much alive,” says Stéphane Hausmann.
Inhibiting without killing
The results of this work show that this regulator affects the production of several virulence factors in the bacteria. “In fact, this protein controls the degradation of numerous messenger RNAs coding for virulence factors”, summarises Martina Valentini. “From an antimicrobial drug strategy point of view, switching off the pathogen’s virulence factors rather than trying to eliminate the pathogen completely, means allowing the host immune system to naturally neutralise the bacterium and potentially reduces the risk for the development of resistance. Indeed, if we try to kill the bacteria at all costs, the bacteria will adapt to survive, which favours the appearance of resistant strains.”
The Geneva team is currently continuing its work by screening a series of known drug molecules in order to determine whether any of them have the capacity to selectively block this protein, and to study in detail the inhibition mechanisms on which the development of an effective therapeutic strategy could be based.
###
Media Contact
Martina Valentini
[email protected]
Original Source
https:/
Related Journal Article
http://dx.