Lysyl oxidase plays several important roles in promoting fibrosis in patients with scleroderma and is a potential biomarker of treatment response
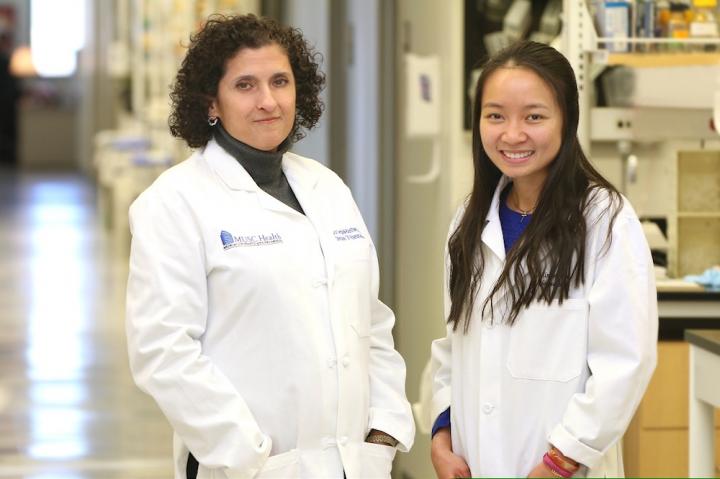
Credit: Sarah Pack, Medical University of South Carolina
A team of researchers at the Medical University of South Carolina (MUSC) has found that the molecule lysyl oxidase (LOX) plays a number of important roles in promoting skin and organ fibrosis in scleroderma, a connective tissue disorder. The researchers have also shown that LOX can be useful in assessing how well an antifibrotic treatment works, suggesting that it may have potential as a biomarker of fibrosis progression or regression.
The team was led by noted fibrosis researcher Carol Feghali-Bostwick, Ph.D., the SmartState and Kitty Trask Holt Endowed Chair for Scleroderma and professor in the Department of Medicine at MUSC, and graduate student Xinh Xinh Nguyen. They report their findings in an article published online ahead of print in the American Journal of Physiology Lung Cellular and Molecular Physiology.
Scleroderma is a connective tissue disease that causes fibrosis, or thickening, of organs such as the lungs, kidneys and heart, along with the skin. In fibrosis, excess connective tissue progressively accumulates around the cells in organs, causing them to lose function and eventually fail. Historically, the only treatment available to these patients has been lung transplantation, which is very invasive and does not stop fibrosis from progressing in other organs. Recently, the Food and Drug Administration approved two new drugs for lung fibrosis, but their usefulness is limited in patients with scleroderma.
“These drugs merely slow the progression of the disease,” said Feghali-Bostwick. “They don’t stop it. They don’t reverse it. New drug targets are urgently needed.”
In the study, Feghali-Bostwick and Nguyen assessed whether LOX might be such a target. They were able to show that LOX plays multiple roles, known as “moonlighting,” in the development and progression of fibrosis in scleroderma. They did so using a preclinical model of lung fibrosis, cells derived from lung and skin tissue samples of patients with scleroderma, and human lung and skin tissue cores. These cores more realistically mimic the physiologic conditions of living human tissue than just growing cells in a petri dish.
Their findings are important because previous research had only shown that LOX increases fibrosis by crosslinking connective tissue. The MUSC team demonstrated that LOX plays additional roles in the progression of fibrosis by stimulating excess production of connective tissue and increasing interleukin 6 (IL-6), an inflammatory molecule.
The research team showed that LOX expression increased 2.8-fold at 10 days following the initiation of lung fibrosis in the preclinical model. The research team also showed that LOX levels and activity were diminished in the lung fibrosis model, almost to baseline levels observed in the control, after administration of an antifibrotic peptide (E4) that is soon to enter a phase 1 clinical trial. These findings suggest that measuring LOX activity in the blood could be a promising biomarker for monitoring treatment response in patients with scleroderma and other fibrotic diseases.
“LOX has a direct role in fibrosis, and measuring circulating LOX levels is useful in monitoring the response to antifibrotic therapies,” said Nguyen, who is a TL1 translational research trainee. The TL1 translational research training program, of which Feghali-Bostwick is the associate director, is funded by the South Carolina Clinical & Translational Research Institute.
Feghali-Bostwick reiterated how important such a biomarker of fibrosis would be.
“It’s exciting that LOX is a biomarker that goes up when we induce lung fibrosis in the mice and goes down when we improve the fibrosis,” she said. “Having a good biomarker of fibrosis would be invaluable because it would allow us to monitor the response to therapy in patients.”
The MUSC team is currently investigating how the E4 peptide reduces fibrosis, not just in the skin and lungs but in other organs as well. Fibrosis is the end-stage of many fibroproliferative diseases that result in organ damage. These include cirrhosis, macular degeneration and cardiovascular disease. If the E4 peptide proves effective at reducing fibrosis in organs beyond the lungs and the skin, it could have potential as an antifibrotic therapy in those patients as well.
This research project was launched by Tetsuya Nishimoto, Ph.D., a postdoctoral fellow in the Feghali-Bostwick laboratory who, in 2016, passed away unexpectedly. Thanks to Nguyen’s efforts, the Feghali-Bostwick laboratory was able to see his project to the end.
###
About MUSC
Founded in 1824 in Charleston, MUSC is the oldest medical school in the South as well as the state’s only integrated academic health sciences center with a unique charge to serve the state through education, research and patient care. Each year, MUSC educates and trains more than 3,000 students and nearly 800 residents in six colleges: Dental Medicine, Graduate Studies, Health Professions, Medicine, Nursing and Pharmacy. The state’s leader in obtaining biomedical research funds, in fiscal year 2019, MUSC set a new high, bringing in more than $284 million. For information on academic programs, visit musc.edu.
As the clinical health system of the Medical University of South Carolina, MUSC Health is dedicated to delivering the highest quality patient care available while training generations of competent, compassionate health care providers to serve the people of South Carolina and beyond. Comprising some 1,600 beds, more than 100 outreach sites, the MUSC College of Medicine, the physicians’ practice plan and nearly 325 telehealth locations, MUSC Health owns and operates eight hospitals situated in Charleston, Chester, Florence, Lancaster and Marion counties. In 2020, for the sixth consecutive year, U.S. News & World Report named MUSC Health the No. 1 hospital in South Carolina. To learn more about clinical patient services, visit muschealth.org.
MUSC and its affiliates have collective annual budgets of $3.2 billion. The more than 17,000 MUSC team members include world-class faculty, physicians, specialty providers and scientists who deliver groundbreaking education, research, technology and patient care.
About the SCTR Institute
The South Carolina Clinical & Translational Research (SCTR) Institute is the catalyst for changing the culture of biomedical research, facilitating the sharing of resources and expertise and streamlining research-related processes to bring about large-scale change in clinical and translational research efforts in South Carolina. Our vision is to improve health outcomes and quality of life for the population through discoveries translated into evidence-based practice. To learn more, visit https:/
Media Contact
Heather Woolwine
[email protected]
Original Source
https:/
Related Journal Article
http://dx.