Stepwise approach enabled telemedicine program to get up and running in three days
Credit: American College of Surgeons
CHICAGO (May 1, 2020): Stay-at-home orders caught many medical practices and health care systems off guard, leaving them ill-equipped to rapidly adopt an efficient telemedicine platform so they could keep providing time-sensitive care to non-COVID-19 patients. To help organizations rapidly introduce telemedicine as an alternative option, a urology group in North Carolina developed a guide that enabled them to convert all in-person visits to telemedicine in three days. They report their experience in an “article in press” appearing on the Journal of the American College of Surgeons website ahead of print.
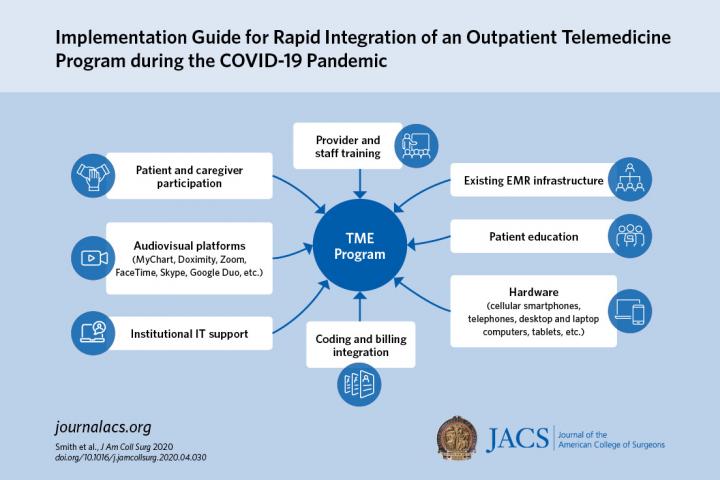
The guide, which the authors call a toolkit, uses a common electronic medical record (EMR) system, Epic, and widely available video portals like Google Duo and Doximity, to overcome social distancing edicts. The toolkit relies on eight essential elements readily available in any medical organization new to telemedicine. “One of our motivations for preparing the toolkit was to make it instantly available to any type of organization, large or small, that has an electronic medical record system,” said lead author Catherine Matthews, MD, FACS, FACOG, professor of urology and gynecology, Wake Forest Baptist Health, Winston-Salem, N.C.
The eight essential components to successful telemedicine adoption are: an existing EMR, a one-hour training session for providers and staff, patient education on accessing the portal, availability of hardware like smartphones and video-capable computers, integration of new billing and coding functions, information technology support, an audiovisual platform, and patient and caregiver buy-in.
“The first thing you have to figure out is which video platform is going to work most consistently,” Dr. Matthews said. Through trial and error, she and her coauthors decided on pairing up the Epic EMR with the Doximity provider networking app. Patients can access the Doximity platform through a link sent in a text message, eliminating the need for them to download an additional app or log into an online portal.
The article acknowledges other options available for telemedicine: the MyChart video capability incorporated in the Epic EMR system, and even services such as FaceTime, Skype, WhatsApp, and Google Duo.
However, in reporting on their experience, the Wake Forest Baptist urology group found disadvantages to some of these alternatives. MyChart, for example, requires patients to sign up for the patient portal and download two separate apps. “It can take quite a bit of time for staff to educate patients about this option,” Dr. Matthews said. “Patients not only have to have the device and Internet access; they have to have enough aptitude to complete those three separate steps.” For providers using their personal devices, platforms like FaceTime and Skype disclose their personal cell phone or e-mail information. Doximity masks that personal contact information with the organization’s office number.
Another key component is the ability to teach both staff and patients quickly how to use the technology. “After selecting the platform, engaging the office staff to be on board with virtual visits is the next most important step,” said coauthor Whitney Smith, MD, a fellow in the female pelvic health service at Wake Forest Baptist Health. Staff training involved a one-hour session with a mock patient visit. The goal, she said, was to replicate all the key steps of the in-person visit in the virtual visit, from front desk check-in and nurse chart review to exam and checkout.
“Telemedicine is currently built as a physician platform,” Dr. Matthews said. “We changed it to be inclusive of nurses; we engaged our nursing staff into the platform so that they continue to do the same roles that they do in person.”
Days before the patient’s telemedicine appointment, a nurse calls to notify the patient the visit is being changed from an in-office to telemedicine, and then walks the patient through the connection process. On the day of the visit, the nurse calls again 15 minutes before the visit to review the chart, “just like they would if the patient was there in the office,” Dr. Matthews said.
About three and a half weeks into their telemedicine experience, the Wake Forest Baptist Health urology physicians see about 15 patient visits via telemedicine a day compared to 30 in-office visits, Dr. Smith added. Despite a lower total number of visits, Dr. Matthews noted that a high rate of new telemedicine patient visits convert to surgery scheduling. “Anecdotally, the efficiency from a surgical subspecialty perspective of the translation of new patient appointments to scheduling of future surgeries is currently 20 to 25 percent,” she said. “So a surgeon who’s not engaging in telemedicine is losing out on an opportunity to identify patients who will need surgery in the next two to three months.”
There have been barriers to wider implementation of telemedicine. Reimbursement for telemedicine services had been one, but in March the Centers for Medicare and Medicaid Services issued a waiver that removed payment restrictions. Another barrier can be technology. Small percentages of people still don’t have smartphones or home computers, and internet service can be limited, especially in some rural areas. Dr. Smith said that the group had concerns about some elderly patients not having access to technology. “However, they’ve been able to engage younger family members to help them with the technology, and actually we’ve had very good success with that,” she said. For patients who don’t have video capability, the CMS waiver accommodates voice-only visits.
###
In addition to Dr. Matthews and Dr. Smith, study coauthors are Anthony J. Atala, MD, FACS; Ryan Terlecki, MD, FACS; and Erin Kelly, MSN, ANP-BC, all with the department of urology at Wake Forest Baptist Health.
The authors have no relevant financial disclosures to report.
“FACS” designates that a surgeon is a Fellow of the American College of Surgeons.
Citation: Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program amidst the COVID-19 Pandemic. Journal of American College of Surgeons.
DOI: https:/
About the American College of Surgeons
The American College of Surgeons is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The College is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an important advocate for all surgical patients. The College has more than 82,000 members and is the largest organization of surgeons in the world. For more information, visit http://www.
Media Contact
Sally Garneski
[email protected]
Related Journal Article
http://dx.




