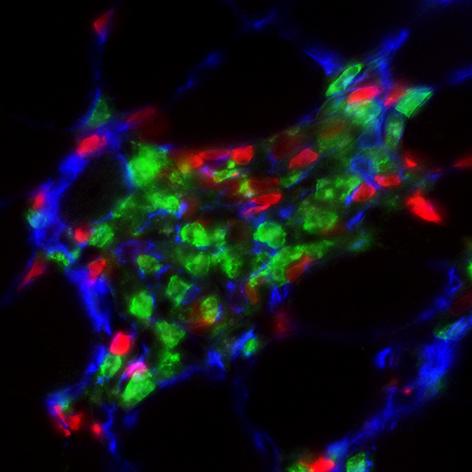
Credit: UCI School of Medicine
Irvine, CA – April 14, 2021 – A new study, led by the University of California, Irvine (UCI), reveals how chronic inflammation promotes muscle fibrosis, which could inform the development of new therapies for patients suffering from Duchenne muscular dystrophy (DMD), a fatal muscle disease.
Titled, “A Stromal Progenitor and ILC2 Niche Promotes Muscle Eosinophilia and Fibrosis-Associated Gene Expression,” the study was published today in Cell Reports.
Chronic inflammation is a major pathological process contributing to the progression and severity of several degenerative disorders, including Duchenne muscular dystrophy (DMD). Studies directed at establishing a causal link between muscular dystrophy and muscle inflammation have revealed a complex dysregulation of the immune response to muscle damage.
During muscular dystrophy, chronic activation of innate immunity causes scarring of skeletal muscle, or fibrosis, compromising motor function. How immunity is linked to the molecular and cellular regulation of muscle fibrosis was not well defined, until now.
“In our study we found the interaction between two types of cells–a novel stromal progenitor, which is similar to a stem cell, and group 2 innate lymphoid cells (ILC2), which are a type of immune cell that reside in skeletal muscle–promotes the invasion of white blood cells in muscle. This condition is associated with the elevation of genes that promote muscle tissue scarring found in DMD,” said lead author Jenna Kastenschmidt, PhD, an assistant specialist in the UCI School of Medicine Department of Physiology & Biophysics.
The new study not only reveals the interaction of cells contributing to DMD, but it illuminates how muscle eosinophilia is regulated. Eosinophils are white blood cells that infiltrate dystrophic muscle causing fibrosis. In this study, researchers found that eosinophils were elevated in DMD muscle compared to control patients. In addition, researchers found the deletion of ILC2s in dystrophic mice mitigated muscle eosinophilia, reducing the expression of genes associated with muscle fibrosis. These findings contribute to the understanding of the complex regulation of muscle inflammation and fibrosis during muscular dystrophy.
“By further defining the interaction between skeletal muscle-resident immune and stromal cells, we can better understand how chronic inflammation promotes muscle fibrosis and, more importantly, we can facilitate development of novel therapies for DMD,” said senior author Armando Villalta, PhD, assistant professor in UCI’s Department of Physiology & Biophysics.
Ongoing work from Villalta’s lab continues to focus on how distinct facets of the immune system regulate DMD pathogenesis and how these processes influence the efficacy and long-term stability of gene replacement therapy.
###
About the UCI School of Medicine
Each year, the UCI School of Medicine educates more than 400 medical students, and nearly 150 doctoral and master’s students. More than 700 residents and fellows are trained at UCI Medical Center and affiliated institutions. The School of Medicine offers an MD; a dual MD/PhD medical scientist training program; and PhDs and master’s degrees in anatomy and neurobiology, biomedical sciences, genetic counseling, epidemiology, environmental health sciences, pathology, pharmacology, physiology and biophysics, and translational sciences. Medical students also may pursue an MD/MBA, an MD/master’s in public health, or an MD/master’s degree through one of three mission-based programs: the Health Education to Advance Leaders in Integrative Medicine (HEAL-IM), the Leadership Education to Advance Diversity-African, Black and Caribbean (LEAD-ABC), and the Program in Medical Education for the Latino Community (PRIME-LC). The UCI School of Medicine is accredited by the Liaison Committee on Medical Accreditation and ranks among the top 50 nationwide for research. For more information, visit som.uci.edu.
Media Contact
Anne Warde
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




