Journal of American College of Surgeons releases new best practice guideline based on potential viral spread patterns, risks facing health care workers, and conservation of personal protective equipment
Credit: American College of Surgeons
CHICAGO (April 6, 2020): Researchers from Stanford University’s department of surgery (Stanford, Calif.) have created an algorithm that aims to protect operating room team members who perform urgent and emergency operations from Coronavirus Disease 2019 (COVID-19) and rationally conserve the personal protective equipment (PPE) they wear. This best practice guideline is published as an “article in press” on the Journal of the American College of Surgeons website ahead of print. Stanford Health Care, verified as a Level 1 trauma center by the American College of Surgeons (ACS), serves Santa Clara and San Mateo Counties, which saw their first cases of COVID-19 infection in early March.
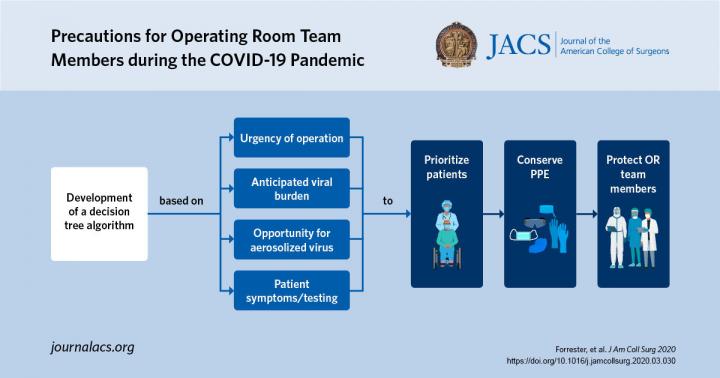
The Stanford algorithm is based on the urgency of the procedure, potential for aerosolization and release of virus droplets at the surgical site, and evidence that a patient has been infected. The algorithm aligns with the goals of the ACS Statement on PPE Shortages during the COVID-19 Pandemic, released April 1, 2020.
“We developed institutional guidelines based on how soon the surgical cases needed to be performed, the patient’s condition, the risk that a surgeon would access an area of body where the amount of virus could be high, and the risk that a patient could be infected with COVID-19,” said Joseph Forrester, MD, MSc, an assistant professor in general surgery and lead author of the algorithm article. Dr. Forrester was a field agent in Liberia during the 2014 Ebola outbreak where he conducted several investigations of the Ebola burden and preparedness as an Epidemic Intelligence Service officer with the Centers for Disease Control and Prevention.
At Stanford, a PPE task force of hospital and medical school leaders from interventional suites, including the operating room, interventional radiology, and endoscopy, as well as quality improvement and infectious disease experts, convened on March 19 to create institutional guidelines that could be implemented within 72 hours. At that time, Stanford Health Care had approximately 10 patients infected with COVID-19. Guidelines incorporated current data about COVID-19 transmission in hospital and non-hospital settings and operating room risk during outbreaks of severe acute respiratory syndrome (SARS) and Ebola.
Patients were triaged by severity of illness into urgent and emergency procedures. Urgent cases were stratified into high- and low-risk procedures depending on the expected viral burden at the surgical site. Procedures categorized as aerosol-generating (AGP) were classified as high-risk. These procedures include those that involve the aerodigestive tract, endoscopy, and open or laparoscopic surgery on the bowel with gross contamination.
The Stanford guideline assumes, above all, that any patient could be infected with COVID-19 unless proven otherwise by a negative RT-PCR test. When operating on COVID-19-postive patients or performing an AGP, the guideline requires operating room team members to be fitted with an N-95 respirator mask and wear a gown, gloves, and eye protection. Only when an RT-PCR test is negative for COVID-19 may surgical team members wear standard surgical clothing.
A surgeon may consider delaying an urgent or emergency procedure on a patient who exhibits viral symptoms (fever, cough, sore throat). If delay compromises the well-being of the patient, the surgeon orders in-house RT-PCR COVID-19 testing with a 24-hour turnaround. If the patient’s status does not allow for a 24-hour wait, the case is considered to be an emergency and the patient is presumed to be COVID-19-positive.
Special considerations are made for the use of PPE during and after bag mask ventilation and endotracheal intubation, which both pose a high risk for viral transmission. All health care providers who are not directly involved with intubation are asked to leave the operating room beforehand. Anesthesiologists should be fitted with N-95 face masks and droplet-protective PPE because they are positioned at the head of the bed throughout the procedure. Cleaning staff should take droplet precautions when cleaning any operating room.
At the time the guideline was created at Stanford Health there was a nationwide shortage of N-95 face masks. To conserve the institution’s supply, the algorithm requires a face shield to be placed over the mask. However, the federal government recently announced that millions of face masks, face shields, surgical masks, gloves, and gowns were entering the medical supply chain, which was encouraging, noted Dr. Forrester.
Dr. Forrester nevertheless recommends that surgical centers where urgent and emergency procedures are performed follow strategies that protect providers and conserve equipment. “You never know what’s going to happen, and it’s better to be prepared and use the right PPE at the right time and be careful not to waste PPE. Guidelines like ours show that health care providers on the frontline are trying to take care of every person with a serious surgical condition and make sure they have enough equipment to carry that mission through safely.”
###
Dr. Forrester’s coauthors are Aussama K. Nassar, MD, MSc, FACS; Paul M. Maggio, MD, MBA, FACS; and Mary T. Hawn, MD, FACS, all from Stanford University’s Department of Surgery.
“FACS” designates that a surgeon is a Fellow of the American College of Surgeons.
The authors have no relevant financial disclosures.
Citation: Precautions for Operating Room Team Members during the COVID-19 Pandemic. Journal of the American College of Surgeons. DOI: https:/
About the American College of Surgeons
The American College of Surgeons is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The College is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an important advocate for all surgical patients. The College has more than 82,000 members and is the largest organization of surgeons in the world. For more information, visit http://www.
Media Contact
Sally Garneski
[email protected]




