NCCN Quality and Outcomes Committee’s endorsements of impactful and feasible quality and outcomes measures offer opportunities to advance the quality of cancer care in America
Credit: JNCCN
PLYMOUTH MEETING, PA [March 10, 2020] — The National Comprehensive Cancer Network (NCCN) has published a curated list of high-impact measures for assessing quality improvements in cancer care. The recommendations reflect a landscape analysis from leading oncology experts; they evaluate measures that, if implemented, will move the needle on cancer care standards in America, with potential implications for policy and coverage. The article, Quality Measurement in Cancer Care: A Review and Endorsement of High-Impact Measures and Concepts, is available via open access in the March 2020 issue of JNCCN–Journal of the National Comprehensive Cancer Network.
The NCCN Quality and Outcomes Committee was first founded in 2016 in order to develop quality and outcome measures in oncology that are:
- more standardized
- contemporary
- clinically relevant
- easily implemented, and
- broadly applicable.
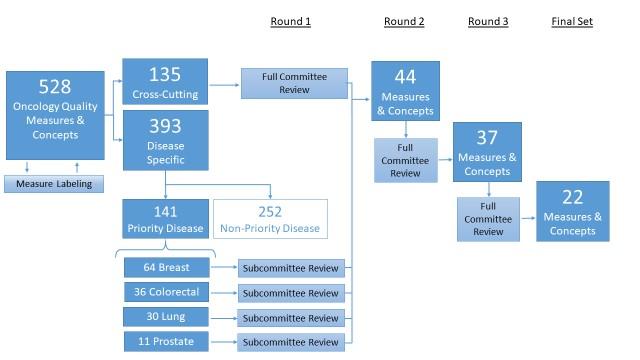
The committee reviewed 528 existing oncology quality measures and new measure concepts that could be appropriate for development. This list was narrowed down into 22 recommendations–based on importance, supporting evidence, opportunity for improvement, and ease of measurement–including endorsement of 15 existing measures and seven new concepts proposed for development.
“The key question underlining all of our efforts is: how can we use quality measurements to improve the experience and outcomes for people with cancer?” said Thomas A. D’Amico, MD, Duke Cancer Institute, Chair of the NCCN Quality and Outcomes Committee. “We reached out to a large number of people including expert clinicians, patient advocates, payers, and health information technology specialists to determine which quality and outcomes measurements would be the most meaningful across the cancer care ecosystem. We paid particular attention to cross-cutting measures that would signify better delivery of care for all different cancer types, while also drilling down into specifics for the highest incidence cancers that affect the most people. These 22 measures represent a feasible standard for documenting quality improvement in cancer care.”
“These recommendations from NCCN differ from certification programs–we are sharing them free-of-charge to allow cancer programs everywhere to be more efficient and focused with their resources while tracking quality improvements,” explained Robert W. Carlson, MD, Chief Executive Officer, NCCN. “There’s a concerted effort toward value-based care; we want to ensure that these payment models reduce costs without reducing quality, and in fact improve outcomes. The current landscape for quality measurements is broad, and it’s difficult to know how to prioritize for quality improvements. This framework from NCCN aligns processes for measuring attainable cancer care improvements that will translate into better outcomes for patients.”
The selected measures are as follows (italics indicates new opportunities for development):
- Across Cancer Types
- Evidence-Based Concordance Measure: Proportion admitted to the intensive care unit (ICU) in the last 30 days of life
- Evidence-Based Concordance Measure: Performance status documented prior to initiating chemotherapy regimen
- Patient Experience Measure: Patients are offered smoking cessation counseling if current smoker
- Treatment Team: Proportion receiving chemotherapy in the last 14 days of life
- Treatment Team: Chemotherapy given within 30 days of end of life
- Treatment Team: Cancer stage documented
- Treatment Team: Proportion dying from cancer in an acute care setting
- Breast Cancer
- Evidence-Based Concordance Measure: Patients with M0 disease, and 4 or more involved axillary lymph nodes, receive breast/chest wall plus regional lymph irradiation as part of their treatment
- Evidence-Based Concordance Measure: Tumor markers are not performed during the period of follow-up surveillance for those who have completed breast cancer treatment with curative intent
- Evidence-Based Concordance Measure: Cardiac function is assessed before starting and at least every 4 months during trastuzumab therapy
- Colorectal Cancer
- Evidence-Based Concordance Measure: For patients with resected pathologic stage 2 and 3 colorectal cancer in surveillance, carcinoembryonic antigen (CEA) is performed at least every 6 months for 5 years
- Evidence-Based Concordance Measure: Patients with rectal cancer are staged with a computed tomography (CT) scan of chest, abdomen, and pelvis and pelvic MRI with contrast or endorectal ultrasound before surgery
- Evidence-Based Concordance Measure: Adjuvant chemotherapy is not administered for patients with pathologic stage 1 colorectal cancer.
- Evidence-Based Concordance Measure: Positron emission tomography (PET) scan is not performed for patients with locoregional colorectal cancer
- Evidence-Based Concordance Measure: Patients with colon cancer are staged with CT scan of chest, abdomen, and pelvis before surgery
- Lung Cancer
- Evidence-Based Concordance Measure: Palliative care consult is offered to patients with metastatic NSCLC within 8 weeks of diagnosis
- Prostate Cancer
- Evidence-Based Concordance Measure: Patients in the high or very-high risk prostate cancer groups, who receive radiation therapy, receive ADT
- Patient Experience Measure: All patients treated with surgery or radiation for localized prostate cancer should be assessed for urinary incontinence and erectile dysfunction with tools such as the UCLA Prostate Cancer Index questions and the Sexual Health Inventory for Men (SHIM)
- Treatment Team: Prostate-specific antigen (PSA) has been measured in the last 12 months for patients with prostate cancer to monitor disease
- Evidence-Based Concordance Measure: Patients with newly diagnosed prostate cancer have a risk group assigned
- Evidence-Based Concordance Measure: Patients in the very low-risk and low-risk prostate cancer groups do not receive androgen deprivation therapy (ADT)
In addition to Drs. D’Amico and Carlson, the NCCN Quality and Outcomes Committee includes:
- Alan Balch, PhD, The National Patient Advocate Foundation
- Lindsey A.M. Bandini, MPH, National Comprehensive Cancer Network
- Al B. Benson III, MD, FACP, FASCO, Robert H. Lurie Comprehensive Cancer Center of Northwestern University
- Stephen B. Edge, MD, FACS, FASCO, Roswell Park Comprehensive Cancer Center
- C. Lyn Fitzgerald, MJ, National Comprehensive Cancer Network
- Robert J. Green, MD, Flatiron Health
- Wui-Jin Koh, MD, National Comprehensive Cancer Network
- Michael Kolodziej, MD, ADVI
- Shaji Kumar, MD, Mayo Clinic Cancer Center
- Neal J. Meropol, MD, Flatiron Health
- James L. Mohler, MD, Roswell Park Comprehensive Cancer Center
- David Pfister, MD, Memorial Sloan Kettering Cancer Center
- Ronald S. Walters, MD, MBA, MHA, MS, The University of Texas MD Anderson Cancer Center
###
Full descriptions of the 22 recommendations, including an explanation of how they each represent important diagnostic and treatment decisions across the continuum of care, can be found at JNCCN.org.
About the National Comprehensive Cancer Network
The National Comprehensive Cancer Network® (NCCN®) is a not-for-profit alliance of 28 leading cancer centers devoted to patient care, research, and education. NCCN is dedicated to improving and facilitating quality, effective, efficient, and accessible cancer care so patients can live better lives. Through the leadership and expertise of clinical professionals at NCCN Member Institutions, NCCN develops resources that present valuable information to the numerous stakeholders in the health care delivery system. By defining and advancing high-quality cancer care, NCCN promotes the importance of continuous quality improvement and recognizes the significance of creating clinical practice guidelines appropriate for use by patients, clinicians, and other health care decision-makers around the world.
The NCCN Member Institutions are: Abramson Cancer Center at the University of Pennsylvania, Philadelphia, PA; Fred & Pamela Buffett Cancer Center, Omaha, NE; Case Comprehensive Cancer Center/University Hospitals Seidman Cancer Center and Cleveland Clinic Taussig Cancer Institute, Cleveland, OH; City of Hope National Medical Center, Duarte, CA; Dana-Farber/Brigham and Women’s Cancer Center | Massachusetts General Hospital Cancer Center, Boston, MA; Duke Cancer Institute, Durham, NC; Fox Chase Cancer Center, Philadelphia, PA; Huntsman Cancer Institute at the University of Utah, Salt Lake City, UT; Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance, Seattle, WA; The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, Baltimore, MD; Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, IL; Mayo Clinic Cancer Center, Phoenix/Scottsdale, AZ, Jacksonville, FL, and Rochester, MN; Memorial Sloan Kettering Cancer Center, New York, NY; Moffitt Cancer Center, Tampa, FL; The Ohio State University Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute, Columbus, OH;
Clinicians, visit NCCN.org. Patients and caregivers, visit NCCN.org/patients. Media, visit NCCN.org/news. Follow NCCN on Twitter @NCCN, Facebook @NCCNorg, and Instagram @NCCNorg.
Media Contact
Rachel Darwin
[email protected]
267-622-6624
Original Source
https:/
Related Journal Article
http://dx.




