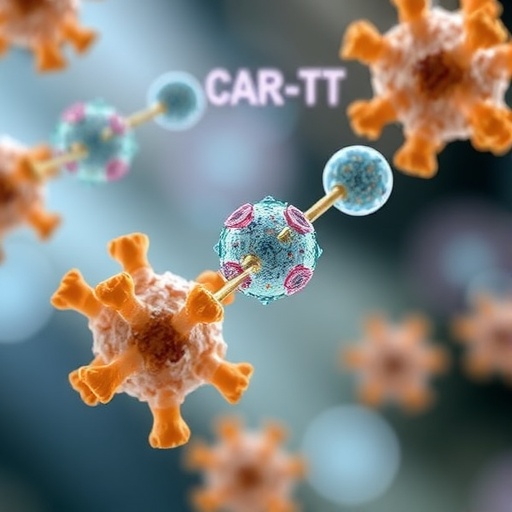
In recent years, the realm of cancer immunotherapy has witnessed revolutionary strides, particularly through the development and clinical success of chimeric antigen receptor T-cell (CAR-T) therapy. This cutting-edge approach reprograms a patient’s own immune cells to identify and eradicate malignant cells with remarkable specificity and potency. However, despite its phenomenal promise, the current CAR-T cell manufacturing process faces significant challenges, including inefficiencies associated with viral vector use, high cost, and limited accessibility. A transformative solution is emerging from the intersection of nanotechnology and cell engineering—nanoparticles. These tiny, engineered particles are poised to redefine CAR-T therapy by facilitating non-viral gene delivery, amplifying in vivo functionality, and even enabling direct in vivo generation of CAR-T cells. This article delves deep into the technical nuances and groundbreaking applications of nanoparticles within CAR-T therapy, offering a glimpse into the future of personalized cancer treatment.
Conventionally, CAR-T cell manufacturing relies heavily on viral vectors—typically lentiviruses or retroviruses—to deliver the CAR transgene into T cells ex vivo. While effective, viral vectors present considerable drawbacks including the risks of insertional mutagenesis, manufacturing complexity, batch variability, and exorbitant costs. Nanoparticle-based delivery systems circumvent many of these issues by offering a versatile, non-viral alternative for gene transfer. Engineered nanoparticles can encapsulate nucleic acids, such as mRNA or DNA plasmids encoding CAR constructs, and facilitate their cellular uptake through endocytosis or membrane fusion. This approach reduces the risk of genomic integration and oncogenic transformation while enabling scalable, reproducible manufacturing processes amenable to widespread clinical deployment.
The design of nanoparticles for CAR gene delivery is a masterful interplay of materials science, immunology, and bioengineering. Lipid nanoparticles (LNPs), inspired by the success of mRNA vaccines, are among the frontrunners due to their biocompatibility, ease of functionalization, and efficient endosomal escape capabilities. These LNPs can be precisely tailored to protect nucleic acids from degradation, enhance cellular uptake by T cells, and ensure release of cargo into the cytosol, where translation or nuclear entry occurs. Additionally, polymeric nanoparticles constructed from biodegradable materials such as poly(lactic-co-glycolic acid) (PLGA) or polyethyleneimine (PEI) offer customizable platforms for controlled gene delivery kinetics, further refining therapeutic efficacy.
.adsslot_A1lC4VIYKj{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_A1lC4VIYKj{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_A1lC4VIYKj{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Beyond gene delivery, nanoparticles can be engineered to serve as immunomodulatory agents that potentiate the in vivo function of CAR-T cells. Tumor microenvironments are notoriously immunosuppressive, deploying physical barriers and biochemical signals that can exhaust or inhibit CAR-T cells. Nanoparticles capable of co-delivering immune-stimulating agents, such as cytokines, checkpoint inhibitors, or metabolic modulators, directly to CAR-T cells or to the tumor milieu can dramatically enhance T cell persistence, proliferation, and cytotoxicity. Moreover, nanoparticles can be functionalized to specifically home to tumor sites or lymphoid organs to localize CAR-T cell activation, thereby minimizing systemic toxicity and off-target effects.
Nonetheless, achieving effective and selective in vivo transfection requires overcoming formidable biological barriers. Circulating nanoparticles must evade immune clearance, resist premature degradation, and traverse complex tissue architectures to reach T cells efficiently. Advances in “stealth” coatings using polyethylene glycol (PEG) and targeting ligands that recognize T cell surface markers (like CD3 or CD8) have shown promise in enhancing nanoparticle biodistribution and cellular specificity. Fine-tuning nanoparticle size, charge, and surface chemistry further optimizes delivery efficiency and therapeutic outcomes.
The safety profile of nanoparticle-based CAR-T therapies is paramount, particularly when considering in vivo applications. Unlike viral vectors, nanoparticles generally exhibit lower immunogenicity and cytotoxicity, reducing adverse immune responses. Nonetheless, off-target effects, unintended gene delivery to non-immune cells, and potential for inflammatory reactions necessitate rigorous preclinical evaluation. Engineering biodegradable nanoparticles that degrade into non-toxic byproducts within controlled timeframes adds an additional layer of safety assurance, ensuring temporary presence within the body.
Integrating nanoparticles with the expanding toolkit of gene editing technologies unlocks unprecedented possibilities for CAR-T cell enhancement. Nanoparticles can simultaneously deliver CRISPR-Cas9 components alongside CAR constructs to achieve site-specific genomic edits that improve CAR expression, prevent immune exhaustion, or confer resistance to immunosuppressive factors within tumors. This combinatorial approach promises CAR-T cells with superior persistence, specificity, and resistance profiles, poised to overcome refractory cancers and heterogeneous tumor landscapes.
Moreover, nanoparticles designed for multimodal imaging capability empower researchers and clinicians with real-time tracking and monitoring of CAR-T cells in vivo. By incorporating contrast agents or fluorescent dyes, nanoparticle platforms can report on biodistribution, expansion dynamics, and tumor infiltration of CAR-T populations. This capability enhances safety monitoring, facilitates dose optimization, and accelerates scientific understanding necessary for clinical translation.
The convergence of nanotechnology and CAR-T therapy is driving a paradigm shift not only in cancer treatment but broadly across cell and gene therapies. The modular nature of nanoparticle engineering allows rapid adaptation to evolving therapeutic targets, logic-gated CAR designs, and combination regimens. As clinical trials begin to validate these approaches, the promise of more accessible, safer, and efficacious CAR-T therapies is becoming an attainable reality rather than a distant aspiration.
In summary, nanoparticles have emerged as indispensable allies in revolutionizing CAR-T cell therapy. Their application spans pivotal facets: enabling non-viral gene delivery that surmounts viral vector limitations, enhancing the in vivo functionality of CAR-T cells within hostile tumor microenvironments, and pioneering the direct in vivo generation of CAR-T cells that democratize access to treatment. Coupled with innovations in gene editing, immunomodulation, and diagnostic imaging, nanoparticle-based strategies stand at the vanguard of a new generation of precision immunotherapies set to transform oncology.
While challenges remain—from optimizing delivery specificity to ensuring regulatory compliance—the momentum is undeniable. As multidisciplinary collaborations surge forward, nanoparticle-enabled CAR-T therapy represents a beacon of hope, promising to extend transformative cancer immunotherapy benefits to patients worldwide with unprecedented safety, efficacy, and convenience.
The future of oncology may well be written in the language of nanoparticles: minuscule vehicles wielding immense therapeutic power to reprogram the immune system and eradicate malignancies at their root. This synthesis of materials science, molecular biology, and clinical medicine exemplifies the extraordinary potential unlocked when frontiers of science collide, illuminating a path toward conquering cancer in ways previously unimaginable.
Subject of Research:
Applications of nanoparticles in CAR-T cell therapy focusing on non-viral gene delivery methods, enhancement of CAR-T cell in vivo efficacy, and in vivo generation of CAR-T cells.
Article Title:
Applications of nanoparticles in CAR-T cell therapy: non-viral manufacturing, enhancing in vivo function, and in vivo generation of CAR-T cells.
Article References:
Albalawi, Y.A. Applications of nanoparticles in CAR-T cell therapy: non-viral manufacturing, enhancing in vivo function, and in vivo generation of CAR-T cells. Med Oncol 42, 378 (2025). https://doi.org/10.1007/s12032-025-02928-6
Image Credits: AI Generated
Tags: CAR-T cell manufacturing challengesefficiency in cell engineeringengineered nanoparticles for T-cell therapyenhancing CAR-T cell performancefuture of cancer immunotherapyinnovations in immunotherapynanoparticles in cancer therapynon-viral gene delivery systemsovercoming viral vector limitationspersonalized cancer treatment advancementstechnical applications of nanotechnology in medicinetransformative solutions in cancer treatment