New study using a rat model for high blood pressure helps explain the different sensory nerve-induced physiological response to air pollution in patients with preexisting cardiovascular disease
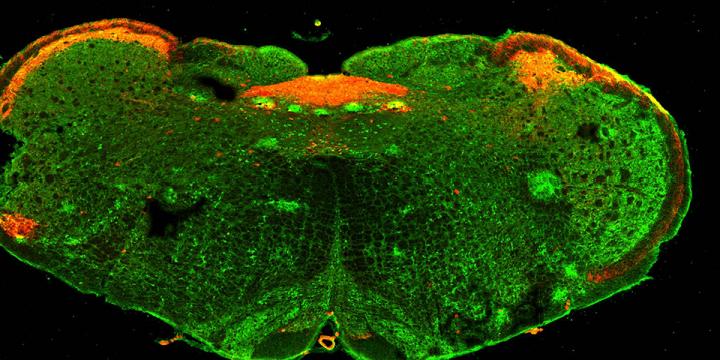
Credit: University of South Florida
TAMPA, Fla. (June 18, 2019) — Air pollution significantly increases the risk for premature deaths, particularly in people with underlying cardiovascular disease, clinical and epidemiological studies have determined.
In healthy people, inhaling ozone or particle pollution triggers a defensive lung-heart reflex (pulmonary-cardiac reflex) that automatically slows heart rate to accommodate oxygen deficiency and help slow distribution of pollutants throughout the body. Yet, when patients with cardiovascular diseases breathe pollutants that same protective mechanism does not kick in. Instead, their heart rates intermittently speed up, known as tachycardia, and can evoke a potentially deadly irregular heart rhythm, known as premature ventricular contractions.
What accounts for the difference? University of South Florida Health (USF Health) researchers who study the role of sensory airway nerves in protective behaviors wanted to know.
Their preclinical findings, reported May 11 in The Journal of Physiology, help explain the altered physiological response to air pollution in patients with preexisting cardiovascular disease.
Using a rat model for high blood pressure (hypertension), a common chronic cardiovascular condition, the USF Health team found that preexisting hypertension altered normal reflexes in the lungs to affect autonomic regulation of the heart when an irritant mimicking air pollution was inhaled. In particular, hypertension appeared to shift the reflex response from the parasympathetic nervous system to the sympathetic nervous system. The sympathetic nervous system mobilizes the body’s defensive “fight-or-flight” response to a threat, including releasing adrenaline that increases heart rate. In contrast, the parasympathetic nervous system controls involuntary responses, including breathing and heart rate, while the body is at rest and maintains a state of calm.
“The speeding up of heart rate and abnormal heart beats (in the hypertensive rats) were due to the switching on of this ‘flight-or-fight’ nervous system not seen in the healthy animals exposed to noxious agents,” said senior author Thomas Taylor-Clark, PhD, associate professor of molecular pharmacology and physiology in the USF Health Morsani College of Medicine. “The heart was responding to an aberrant nerve-generated reflex that may worsen preexisting cardiovascular disease.”
To simulate effects of air pollution inhaled into the lungs — difficult to recreate in a laboratory setting — the USF researchers used allyl isothiocyanate, the pungent ingredient in wasabi and horseradish. When healthy rats with normal blood pressure inhaled this irritant, their heart rates slowed as expected. But, in the rats with chronic hypertension, inhaling the same irritant stimulated an increased heart rate accompanied by premature ventricular contractions.
Surprisingly, a rapid heart rate and abnormal heart rhythm did not occur when allyl isothiocyanate was intravenously injected into the hypertensive rats.
“It did not evoke the peculiar reflex; instead, we observed a slowing of the heart rate like that seen in the rats with normal blood pressure,” Dr. Taylor-Clark said. “This suggests that the sensory airway nerves accessible by IV are different than those accessible by inhalation… so perhaps the pathways of airway sensory nerves (connecting organs like the heart and lungs with the brainstem,) are more complex than previously understood.”
Chronic hypertension may remodel airway sensory nerves controlling the pulmonary-cardiac reflex that helps defend the body against physical damage from air pollution, the USF study suggests. This remodeling, which may happen in the developmental stages of hypertension, could turn on inappropriate sympathetic nervous system excitation of the heart, Dr. Thomas-Taylor said.
By better understanding how cardiovascular disease changes neuronal interactions between the heart and lungs, the researchers hope to help doctors with treatment choices – and eventually discover new treatments.
“Our goal is to add another piece of information that clinicians could consider when selecting a best treatment for hypertension. In addition to the patient’s age, ethnicity and race, that might include whether the person lives in an area with high pollution levels,” he said. “In the long-term, if we can identify the nervous system mechanisms involved in remodeling the pulmonary-cardiac reflex, we can target those to develop new blood pressure drugs.”
###
The USF Health study was supported by grants from the American Heart Association, the National Institutes of Health’s National Heart, Lung and Blood Institute, and the NIH Commonfund.
More than four in 10 Americans are at risk of disease and premature death due to air pollution, the American Lung Association reports. And, more than one-third of the deaths from lung cancer, heart disease and stroke are associated with air pollution, according to the World Health Organization.
USF Health’s mission is to envision and implement the future of health. It is the partnership of the USF Health Morsani College of Medicine, the College of Nursing, the College of Public Health, the College of Pharmacy, the School of Physical Therapy and Rehabilitation Sciences, the Biomedical Sciences Graduate and Postdoctoral Programs, and the physicians of USF Health, the largest multispecialty group practice on Florida’s west coast. The University of South Florida, established in 1956 and located in Tampa, is a high-impact, global research university dedicated to student success. USF ranks in the top 25 nationally for research expenditures among public universities, according to the National Science Foundation.
Media Contact
Anne DeLotto Baier
[email protected]
Original Source
https:/
Related Journal Article
http://dx.