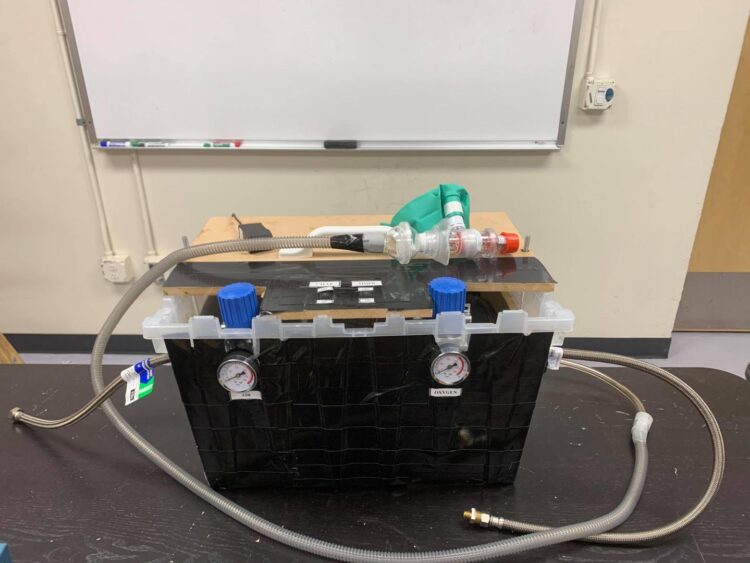
Researchers are developing simple and inexpensive tools–like a DIY ventilator–to treat patients more effectively and prevent disease transmission in hospitals
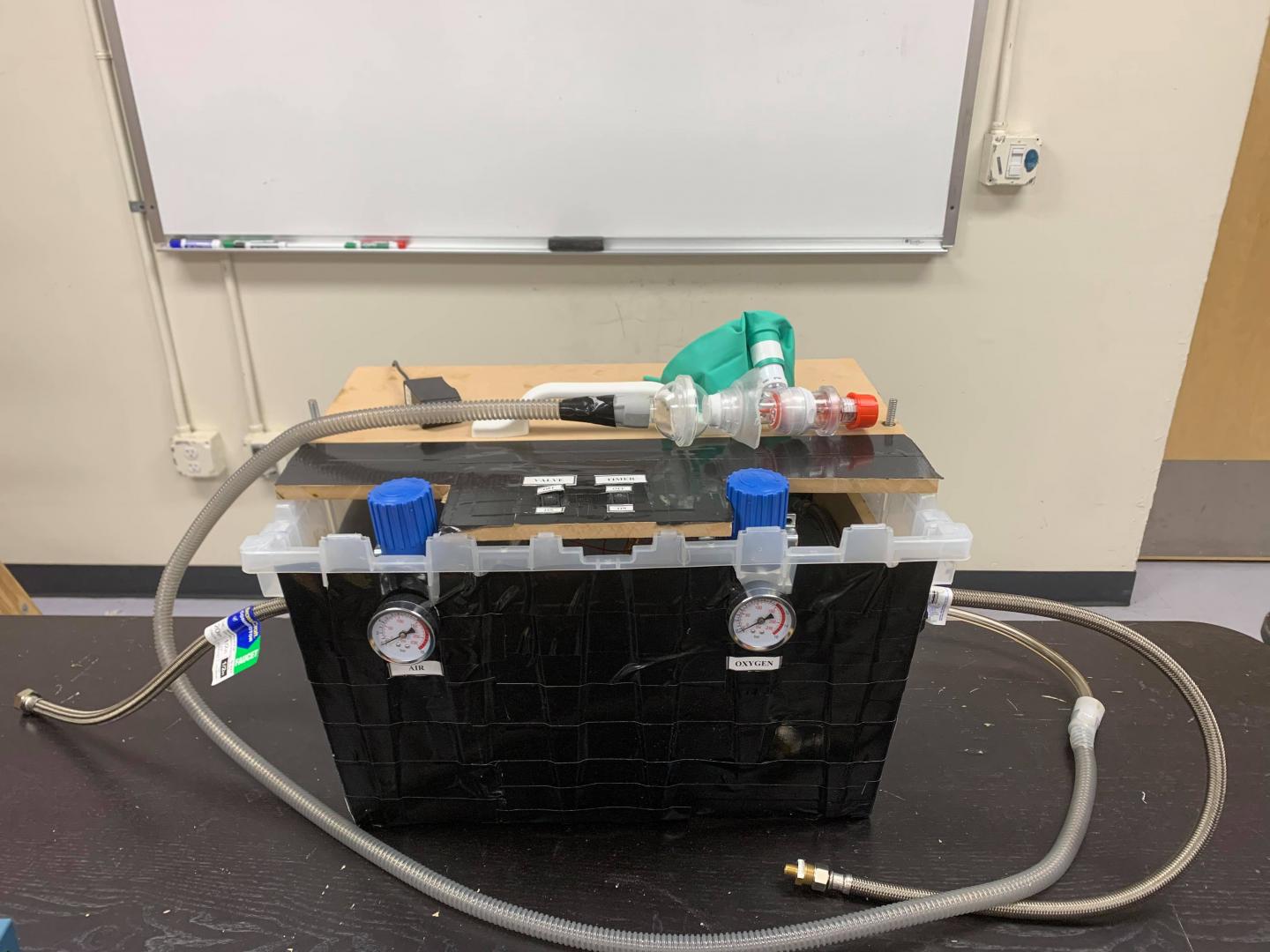
Credit: Mohamed Amine Abassi.
VIRTUAL MEETING (CST), November 22, 2020 — The rapid spread of COVID-19 overwhelmed hospitals that were unable to contend with the increasing number of patients, many requiring ventilators and other critical care. Such conditions can put medical workers at risk. Now researchers are studying methods to increase hospital safety and efficacy during the pandemic.
A shortage of life-saving ventilators, which typically cost around $30,000 each, hit hospitals particularly hard.
“By building a simple and cheap ventilator, we can help alleviate this burden for the medical staff,” said Mohamed Amine Abassi, a PhD student in fluid mechanics.
Based on a prototype designed by his advisor, engineering professor Xiaofeng Liu, Abassi spearheaded an effort with colleagues from San Diego State University and the University of California San Diego to build such a device from readily available parts–plastic tubing, pressure valves, humidifier–and an air supply. Then they tested it.
Preliminary results shared at the 73rd Annual Meeting of the American Physical Society’s Division of Fluid Dynamics suggest the ventilator meets essential requirements set by the Food and Drug Administration. It is fully controllable on three parameters–air pressure, inspiration time, and Positive End Expiratory Pressure (PEEP)–with plans for more controls in the works.
Abassi and Liu foresee the ventilators assisting not just overwhelmed hospitals in the United States but also in developing countries and rural areas with limited medical infrastructure. “If they can build it at home, they can use it,” said Abassi. “And you can build many of these ventilators in a very short time.”
Patients on ventilators who have some pulmonary conditions relevant to COVID-19 with underlying chronic lung diseases will often receive drugs like albuterol through an endotracheal tube. This treatment relaxes the bronchial muscles and improves airflow to the constricted lung airways.
A group from Lehigh University and the University of Arkansas for Medical Sciences sought the most effective methods for administering albuterol via ventilator.
Ariel Berlinski and his group conducted aerosol characterization experiments at the University of Arkansas. Rahul Rajendran at Lehigh used the results to investigate drug delivery through computations.
“The research objective was to evaluate the efficiency of drug delivery when the nebulizer type and its placement were varied in the ventilator circuit,” said Arindam Banerjee, a member of the group and a Lehigh professor of mechanical engineering and mechanics.
The researchers found that a vibrating mesh (rather than a jet) nebulizer placed on the dry side of the humidifier delivers the highest dose to the lung. Administering albuterol through intubation works most effectively for smaller particles, while oral administration is more efficient for larger particles.
“Our results are vital for mechanical ventilator based treatment,” said Banerjee.
Even in optimal circumstances, healthcare workers still risk contracting COVID-19. A new respiratory apparatus could reduce exhaled aerosols, which are known to transmit the virus that causes the disease.
Researchers from Liberty University and Vapotherm wondered how common respiratory treatments would affect aerosol emissions. So they decided to test a proposed design for a PVC face mask connected to suction, adding a high-velocity nasal insufflation cannula–the kind of tubed device that delivers oxygen to the nose.
Then, with input from medical experts, they modeled a hospital room with two patients and four caregivers using highly sophisticated computational techniques. According to their model, when patients wear the new apparatus, fewer particles reach the healthcare workers.
“It represents an inexpensive way to reduce the spread of airborne contagion using supplies commonly found in hospital rooms already,” said engineering PhD candidate Reid Prichard. “This will remain an important tool even after the pandemic is over.”
Another group from the University of South Florida, led by mechanical engineering PhD student Anthony Perez, is investigating what happens to any aerosol contaminants that patients do emit into a hospital isolation room–and how quickly the contaminants leave the room.
“As many hospitals are reaching capacity, ensuring a hospital room is safe to enter after an aerosol-generating procedure–or after the removal of a previous patient so hygiene workers can prepare the room–requires significant down time,” said Perez.
According to the researchers, the Centers for Disease Control and Prevention ventilation recommendations assume pathogen-containing aerosols are perfectly mixed within a room. Using numerical simulations, the group finds that imperfect mixing conditions significantly affect how quickly ventilation removes pathogens from a room.
“It is both surprising and somewhat concerning that the standard for air sanitization is based on what many would consider a back-of-an-envelope calculation,” said Perez.
The simulations suggest aerosol contaminants can linger in “dead zones” for around 10 minutes in a typical hospital isolation room. Meanwhile, “short circuits” expel some packets of contaminants quickly before they can disperse.
“Our research illustrates the need for a more accurate, yet inexpensive, framework for the prediction of aerosol concentrations in an arbitrary hospital room, especially in assessing the level of exposure of healthcare workers,” said Perez.
###
HIGHLIGHTED ABSTRACTS
Design, Build and Test of an In-House Made Ventilator System
POSTER: 11:30 a.m. CST, Tuesday, November 24, 2020
ABSTRACT: http://meetings.
CONTACT: Xiaofeng Liu, [email protected]
Albuterol Delivery Through An Adult Ventilator Circuit To A Patient-Specific Tracheobronchial Airway Model
POSTER: 5:45 p.m. CST, Sunday, November 22, 2020
ABSTRACT: http://meetings.
CONTACT: Rahul Rajendran, [email protected] Arindam Banerjee, [email protected]
Novel Use of a Common Respiratory Treatment: Diminishing COVID-19 Transmission
POSTER: 3:55 p.m. CST, Sunday, November 22, 2020
ABSTRACT: https:/
CONTACT: Wayne Strasser, [email protected] and Reid Prichard, [email protected]
Numerical Investigation of the Role of Air Ventilation Rate in Reducing Healthcare Worker Exposure to Infectious Aerosols in a Hospital Isolation Room
POSTER: 10:00 a.m. CST, Tuesday, November 24, 2020
ABSTRACT: http://meetings.
CONTACT: Anthony Perez, [email protected]
USEFUL LINKS
Meeting Website: https:/
Scientific Program: https:/
Registration: https:/
Complimentary registration is available to credentialed media for the express purpose of gathering and reporting news and information from the meeting. If you have not previously obtained APS press credentials (i.e. attended other APS meetings as press or receive the APS journals tip sheet), please submit a request at http://info.
ABOUT DFD
The Division of Fluid Dynamics of the American Physical Society, established in 1947, exists for the advancement and diffusion of knowledge of the physics of fluids with special emphasis on the dynamical theories of the liquid, plastic, and gaseous states of matter under all conditions of temperature and pressure.
ABOUT APS
The American Physical Society (APS) is a nonprofit membership organization working to advance and diffuse the knowledge of physics through its outstanding research journals, scientific meetings, and education, outreach, advocacy, and international activities. APS represents over 55,000 members, including physicists in academia, national laboratories, and industry in the United States and throughout the world. Society offices are located in College Park, Maryland (Headquarters), Ridge, New York, and Washington, DC.
Media Contact
APS Press Office
[email protected]