The groundbreaking study led by researchers Corroenne, Sanz Cortes, and Whitehead sheds light on a critical aspect of prenatal care by exploring the intricacies of hindbrain herniation severity grading. This complex condition, which is often encountered in fetuses with neural tube defects, has significant implications for both diagnosis and treatment outcomes. With the advent of advanced imaging techniques like MRI, the necessity for accurate and reproducible grading systems has never been more paramount. The work unfolds new methodologies and understanding of the grading process, which could reshape prenatal interventions and improve long-term health outcomes for affected fetuses.
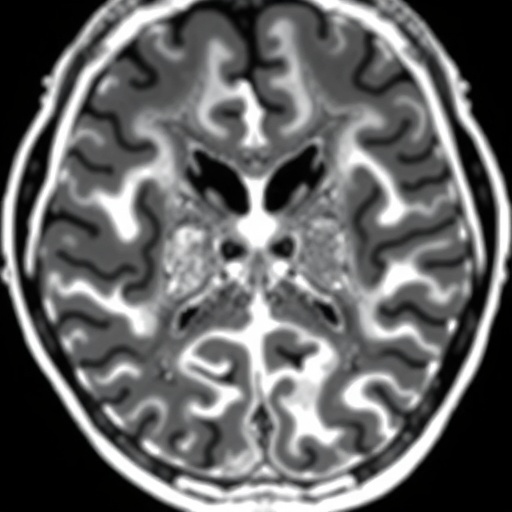
In this extensive research, the authors meticulously examine the reproducibility of grading hindbrain herniation severity through MRI scans. As professionals in the field of pediatric radiology, they recognize the critical need for precise diagnostic tools that can facilitate early interventions and improve clinical decision-making. The study underscores how variations in grading can lead to different interpretations which, in turn, could influence treatment protocols and prognostic assessments. Ensuring consistency in this grading process is foundational to prenatal care, especially as more expectant parents are being informed of potential neural tube defects.
The researchers employed a rigorous methodological framework, analyzing MRI scans of fetuses who underwent prenatal open neural tube defect repair. Each case was meticulously graded, with special attention to the features of hindbrain herniation. By comparing results among different evaluators, the team was able to gauge the inter-rater reliability of the grading system deployed. Importantly, the study emphasizes how discrepancies in interpretations could significantly affect the clinical management of these pregnancies, highlighting the urgent need for standardized protocols in this area.
One of the study’s major highlights is its focus on the role of MRI as a prominent imaging modality in understanding fetal anatomy and potential complications. While ultrasound has been the traditional method for prenatal evaluations, MRI offers enhanced visualization of cranial structures, particularly in complex conditions like open neural tube defects. This allows clinicians to make more informed decisions regarding surgical interventions, ultimately aiming to reduce fetal and neonatal morbidity. The findings herein suggest that MRI not only assists in diagnosis but also plays an instrumental role in pre-surgical planning and subsequent management.
The researchers also delve into the implications of standardized grading on clinical outcomes. With an accurate grading system, healthcare providers can better stratify risk and allocate resources wisely. For instance, fetuses diagnosed with severe hindbrain herniation can be flagged for more intensive monitoring and earlier reparative procedures. This timely springboard into clinical action could lead to reductions in post-operative complications and better overall survival rates. The quest for reproducibility thus emerges as a linchpin for improving care pathways for both providers and patients.
Interestingly, the assessment of hindbrain herniation severity includes not just anatomical measurement but also the functional impacts of the condition on fetal development. The study articulates how hindbrain herniation alters cerebrospinal fluid dynamics, which in turn can have cascading effects on brain development. Understanding these relationships will be vital as clinicians consider the broader implications of surgical interventions. Insights from this study can contribute to a more nuanced understanding of how to navigate challenges associated with neural tube defects.
Though the research presents optimistic possibilities, it also calls for caution. The authors emphasize that while their findings are promising, further validation within larger cohorts is crucial for generalizability. Rigorous testing of the proposed grading criteria across diverse populations can solidify its applicability and reliability. Contextual factors such as genetic background and environmental influences may significantly impact fetal development and health outcomes, creating a need for ongoing research to address these variables.
The implications for ethical discussions in prenatal care are profound as well. When parents are informed of risks associated with hindbrain herniation severity, it necessitates sensitive conversations around therapeutic interventions and potential outcomes. The study reevaluates how pediatric practitioners approach these discussions, providing a tangible grading system that can facilitate clearer communication. This transparency holds potential for empowering parents, allowing them to engage actively in decision-making pertaining to their unborn child’s health.
As the conversation around health equity grows, this research also reflects the critical need to implement standardized protocols that are accessible across various healthcare settings. Not all prenatal care providers have the same access to advanced imaging techniques, and disparities in healthcare can hinder equitable access to optimal care. The study advocates for collaboration among different institutions to harness resources effectively and spread the benefits of such advancements uniformly. A more unified approach can help bridge the discrepancies that exist within prenatal care, minimizing variation in practices that could affect outcomes.
Moreover, as we witness rapid advancements in technology, the research opens doors for integrating machine learning and artificial intelligence into the grading process. These innovations can potentially enhance the accuracy of severity assessments and provide comprehensive analyses of MRI data. Such synergies between innovative technology and traditional healthcare practices could yield an era of unprecedented enhancements in diagnostic accuracy and treatment efficacy.
In conclusion, the research by Corroenne et al. marks a pivotal milestone in pediatric radiology and prenatal care, redefining the standards for grading hindbrain herniation severity. The meticulous approach demonstrated reveals the significance of upholding reproducibility in clinical assessments, which can directly impact patient care. As healthcare providers consider these findings, the hope is for a future where standardized and reproducible methodologies become a hallmark of improved prenatal interventions.
The call to action is clear: as we progress in addressing these complex conditions, our focus must remain on fostering collaboration across specialties and adopting rigorous protocols that emphasize reproducibility. This collaborative spirit not only benefits healthcare providers but also empowers families by ensuring that they receive the best-informed care possible for their unborn children.
Ultimately, the study encourages a collective push toward redefining prenatal assessments, reiterating the importance of research in shaping clinical practices and improving health outcomes. As the field stands on the brink of transformative shifts, embracing such advancements will be essential in the ongoing journey toward excellence in prenatal medicine.
Subject of Research: Hindbrain herniation severity grading in fetuses undergoing prenatal open neural tube defect repair.
Article Title: Reproducibility of hindbrain herniation severity grading on MRI scan in fetuses undergoing prenatal open neural tube defect repair.
Article References:
Corroenne, R., Sanz Cortes, M., Whitehead, W. et al. Reproducibility of hindbrain herniation severity grading on MRI scan in fetuses undergoing prenatal open neural tube defect repair.
Pediatr Radiol (2026). https://doi.org/10.1007/s00247-025-06499-6
Image Credits: AI Generated
DOI: 09 January 2026
Keywords: Hindbrain herniation, MRI, prenatal care, neural tube defects, reproducibility, pediatric radiology, fetal health, ethical considerations, healthcare equity.
Tags: diagnosis and treatment of fetal conditionsearly interventions for affected fetusesfetal MRI imaging techniquesgrading systems for fetal abnormalitieshindbrain herniation gradingimplications of MRI in prenatal interventionsimproving clinical decision-making in prenatal carelong-term health outcomes in prenatal diagnosispediatric radiology advancementsprenatal care for neural tube defectsreproducibility in medical diagnosticsunderstanding hindbrain herniation severity