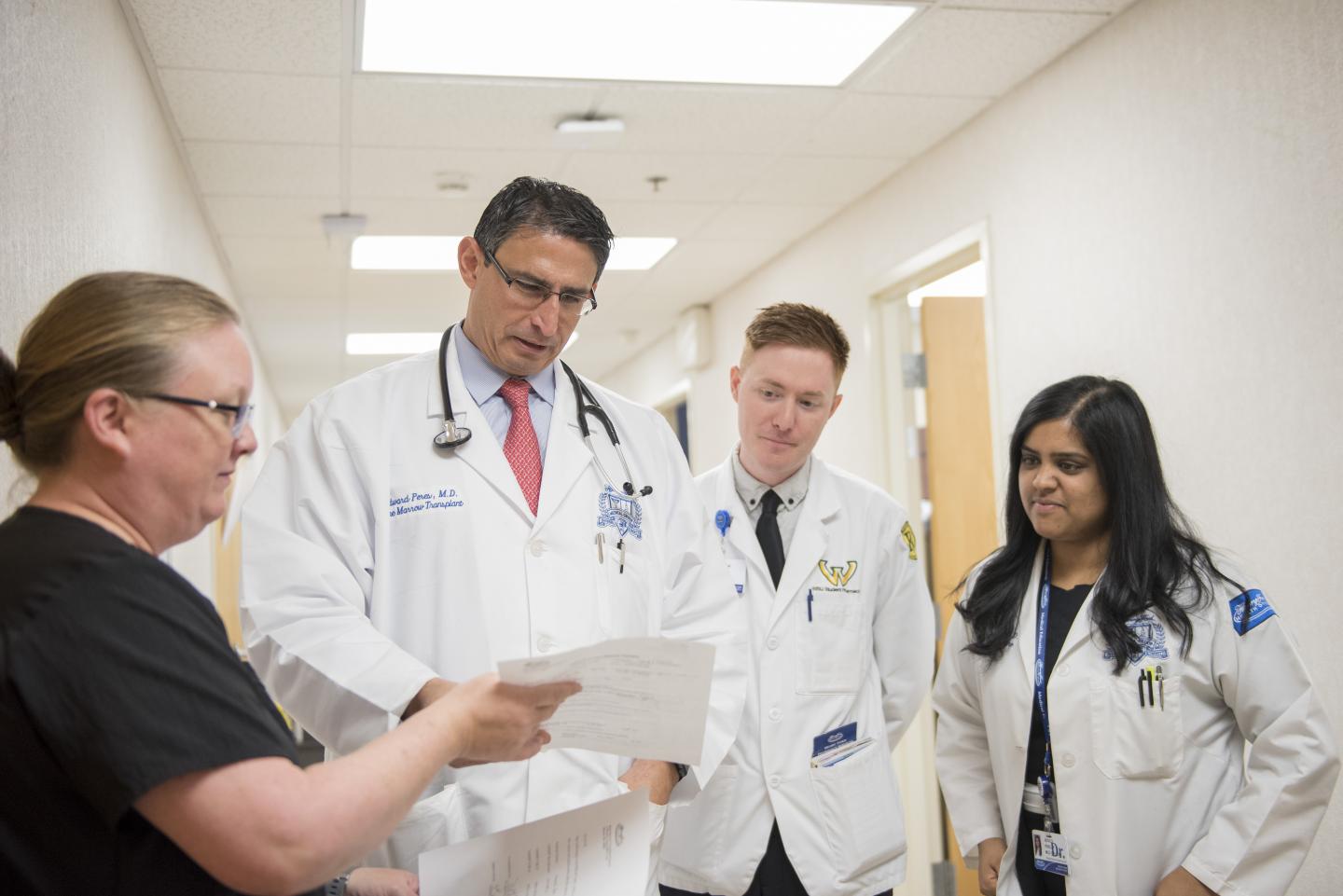
Credit: Henry Ford Health System
DETROIT – Henry Ford Cancer Institute has treated its first patient with CAR T-cell therapy, an approach that uses engineered cells from a patient’s immune system to destroy cancer. The altered cells remain active for years after the treatment, acting as a “living drug.”
Only specially-certified trained hospitals can offer CAR T-cell therapy to patients with B-cell acute lymphocytic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). Henry Ford is one of them, and a Southeast Michigan woman is the health system’s first patient.
“When patients are told ‘nothing else can be done,’ and they hear that CAR T-cell therapy may be an option, they are going to be very excited,” says Edward M. Peres, M.D., medical director of the CAR T-Cell Program at Henry Ford Cancer Institute.
The National Cancer Institute estimates that in 2019, an estimated 5,930 people in the U.S. will have ALL, a cancer of the blood and bone marrow. Each year, approximately 3,100 new patients aged 20 or younger are diagnosed with ALL. The disease is also known as acute lymphoblastic leukemia. “Acute” means that the disease can progress quickly, resulting in death within a few months if it is not treated.
“Without this therapy, patient survival would be less than 10 percent,” says Dr. Peres.
The therapy is approved by the U.S. Food and Drug Administration for pediatric and young adult patients who have ALL, and for adult patients with DLBCL that has relapsed or is difficult to treat. CAR T-cell therapy is available only at a few hospitals in Michigan that have special certification.
“Ours is a program with more personalized care. We have top experts in lymphoma and leukemia, so patients can feel confident they will have a team that can manage an untreatable cancer and hopefully get some response and possibly a cure,” Dr. Peres.
For patients with DLBCL that has relapsed or has not responded to other treatments, the first FDA-approved CAR T-cell therapy, tisagenlecleucel, showed a relapse-free survival of 65% at 12 months. CAR T-cell gene therapy is a one-time treatment at the forefront of precision medicine. Henry Ford Cancer Institute’s Bone Marrow Transplant program, a joint effort by the bone marrow transplant physicians and staff, is critical to the success of CAR T-cell therapy.
“We are utilizing the patient’s cells and manufacturing a specific immune therapy for them,” says Dr. Peres. “Instead of chemotherapy that treats the whole body and is hopefully killing the cancer, we’re treating the cancer with targeted and precision medicine using the patient’s immune system.”
CAR T-cell therapy involves several steps:
- T-cells are removed from the patient in a process similar to donating blood. After the cells have been separated from the blood, the blood is immediately returned to the body.
- The pharmaceutical company’s manufacturing lab inserts a new gene into the T-cells with instructions to make and add a new protein to their surface. That protein is called a chimeric antigen receptor (CAR).
- While the CAR T-cells are multiplying in the laboratory, the patient may remain out of the hospital and may receive a brief course of outpatient chemotherapy.
- When millions of CAR T-cells have been grown – this may take a few weeks – the cells are frozen and delivered to the hospital where they are infused into the patient. The CAR T-cells will continue to multiply in the patient and attack cancer cells, working as a “living drug.”
One of the challenges with CAR T-cell therapy is the side effects. Many patients have severe flu-like symptoms as the T-cells fight cancer. Some people may experience confusion or additional neurological symptoms that can be reversible. Other side effects can be more serious. To evaluate and treat those side effects, the patient remains in the hospital for two or more weeks.
“Patients can rest assured that they will be closely monitored in a transplant unit and/or intensive care unit, and will be provided medications for any side effects,” says Dr. Peres. “We do everything possible for these patients.”
Likewise, the detailed management process begins during a patient’s first visit when a multidisciplinary team evaluates everything from past medical to possible medical scenarios, psychological areas and even insurance coverage. Each patient also has a designated nurse navigator and financial coordinator.
“We make it very easy for the patient. All they have to do is show up,” says Dr. Peres.
###
To learn more or request an appointment, visit henryford.com/cancer or call (888) 777-4167.
Media Contact
Jeff Adkins
[email protected]
Original Source
https:/




