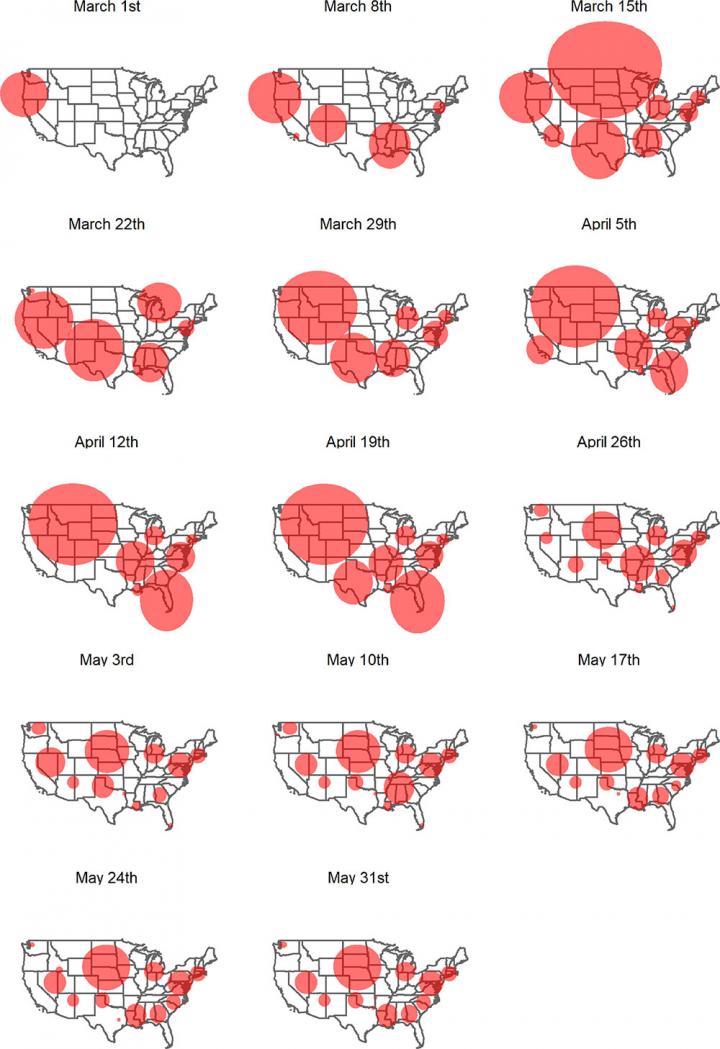
Hotspots have trended towards smaller but more numerous clusters since the pandemic started
Credit: Hohl et al., Spatial and Spatio-temporal Epidemiology (2020)
Over the course of the coronavirus epidemic, COVID-19 outbreaks have hit communities across the United States. As clusters of infection shift over time, local officials are forced into a whack-a-mole approach to allocating resources and enacting public health policies. In a new study led by the University of Utah, geographers published the first effort to conduct daily surveillance of emerging COVID-19 hotspots for every county in the contiguous U.S. The researchers hope that timely, localized data will help inform future decisions.
Using innovative space-time statistics, the researchers detected geographic areas where the population had an elevated risk of contracting the virus. They ran the analysis every day using daily COVID-19 case counts from Jan. 22 to June 5, 2020 to establish regional clusters, defined as a collection of disease cases closely grouped in time and space. For the first month, the clusters were very large, especially in the Midwest. Starting on April 25, the clusters become smaller and more numerous, a trend that persists until the end of the study.
The article published online on June 27, 2020, in the journal Spatial and Spatio-temporal Epidemiology. The study builds on the team’s previous work by evaluating the characteristics of each cluster and how the characteristics change as the pandemic unfolds.
“We applied a clustering method that identifies areas of concern, and also tracks characteristics of the clusters–are they growing or shrinking, what is the population density like, is relative risk increasing or not?” said Alexander Hohl, lead author and assistant professor at the Department of Geography at the U. “We hope this can offer insights into the best strategies for controlling the spread of COVID-19, and to potentially predict future hotspots.”
The research team, including Michael Desjardins of Johns Hopkins Bloomberg School of Public Health’s Spatial Science for Public Health Center and Eric Delmelle and Yu Lan of the University of North Carolina at Charlotte, have created a web application of the clusters that the public can check daily at COVID19scan.net. The app is just a start, Hohl warned. State officials would need to do smaller scale analysis to identify specific locations for intervention.
“The app is meant to show where officials should prioritize efforts–it’s not telling you where you will or will not contract the virus,” Hohl said. “I see this more as an inspiration, rather than a concrete tool, to guide authorities to prevent or respond to outbreaks. It also gives the public a way to see what we’re doing.”
The researchers used daily case counts reported in the COVID-19 Data Repository from the Center for Systems Science and Engineering at Johns Hopkins University, which lists cases at the county level in the contiguous U.S. They used the U.S. Census website’s 2018 five-year population estimates within each county.
To establish the clusters, they ran a space-time scan statistic that takes into account the observed number of cases and the underlying population within a given geographic area and timespan. Using SatScan, a widely used software, they identified areas of significantly elevated risk of COVID-19. Due to the large variation between counties, evaluating risk is tricky. Rural areas and small, single counties may not have large populations, therefore just a handful of cases would make risk go up significantly.
This study is the third of the research group’s iteration using the statistical method for detecting and monitoring COVID-19 clusters in the U.S. Back in May, the group published their first geographical study to use the tracking method, which was also of the first paper published by geographers analyzing COVID-19. In June, they published an update.
“May seems like an eternity ago because the pandemic is changing so rapidly,” Hohl said. “We continue to get feedback from the research community and are always trying to make the method better. This is just one method to zero in on communities that are at risk.”
A big limitation of the analysis is the data itself. COVID-19 reporting is different for each state. There’s no uniform way that information flows from the labs that confirm the diagnoses, to the state health agencies to the COVID-19 Data Repository from the Center for Systems Science and Engineering at Johns Hopkins University, where the study gets its data. Also, the testing efforts are quite different between states, and the team is working to adjust the number of observed cases to reflect a state’s efforts. Hohl is also working with other U researchers to look at the relationship between social media and COVID-19 to predict the future trajectory of outbreaks.
“We’ve been working on this since COVID-19 first started and the field is moving incredibly fast,” said Hohl. “It’s so important to get the word out and react to what else is being published so we can take the next step in the project.”
###
Media Contact
Lisa Potter
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




