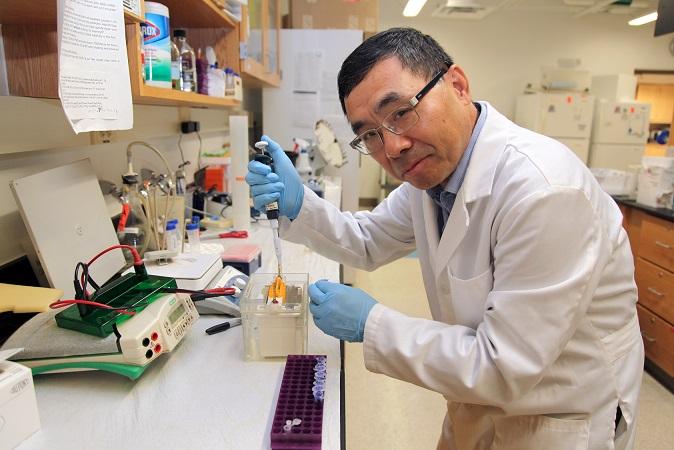
Credit: Kim Ratliff, Production Coordinator, Augusta University
Dr. Guangyu Wu is dissecting the molecular homing that enables a nascent protein to ultimately find its way to the surface of a cell as a mature receptor type that helps us taste, smell and even regulate our mood and immunity.
“These receptors are essential for normal body function, many diseases use them and many drugs target them,” says Wu, pharmacologist in the Department of Pharmacology and Toxicology at the Medical College of Georgia at Augusta University.
Wu is talking about G protein-coupled receptors, or GPCRs, that with more than 800 types in the human genome, are the largest of three classes of cell surface receptors involved in an also large number of essential functions and targeted by at least a third of the drugs out there for common problems like heart failure, diabetes, Parkinson’s and Alzheimer’s.
He’s principal investigator on a $1.7 million grant (1R35GM136397-01) from the National Institute of General Medical Sciences to help determine the molecular mechanisms that enable a mature GPCR to reach the surface of our cells, both to better understand this continuous, fundamental physiological process, and how to optimize the use of hormones and drugs we give to target those receptors.
The GPCRs Wu is using are the adrenergic receptors. These are highly expressed on cells like neurons as well as our blood vessels and kidneys, and regulate the sympathetic nervous system, which regulates the body’s fight or flight response, to do things like temporarily increase our heart rate and blood pressure so we can run from danger, and inhibit things like digestion so we can focus on fighting or fleeing. These receptors are natural targets for the hormone adrenaline and neurotransmitter noradrenaline, but manmade drugs like beta-blockers mimic these endogenous ligands that bind to these receptors to activate or block their action.
An early production point for making adrenergic and other GPCRs is the endoplasmic reticulum, which is like a protein manufacturing plant inside our cells, where, in this case, long proteins are made and folded that should eventually become GPCRs. The nearby Golgi apparatus is like the finishing plant that helps modify, package and put proteins as well as lipids in the correct taxi before their debut as receptors on the cell surface.
As the protein makes its way out of the endoplasmic reticulum, Wu has watched how it catches a ride, called a vesicle, a tiny compartment that travels inside our cells. The protein stops periodically to emerge from one vesicle, be further modified, then request and catch another newly assembled vesicle — the previous ride moves into the Golgi — then move on in a journey that includes several moves and may take up to an hour, Wu says. From the start of protein formation to the surface can actually take more like 20 hours all told. The process is nonstop in our bodies, and although the exact shelf life of a GPCR is not known, it is known that receptors are constantly arriving on the cell surface while existing ones move back inside the cell to be degraded.
Wu already has some evidence of the essential role of ufymylation, an also ongoing body process when the small protein UFM1 attaches to another protein to modify its function, and the key protein players C1orf27, GGA3 and HCR1, in a GPCR’s journey.
One of the many questions Wu is working to answer now is how and when ufmylation and this protein C1orf27 influence formation of a receptor and moving the budding receptor from the endoplasmic reticulum to the Golgi apparatus for fine-tuning. He also wants to know what HCR1 and GGA3 do in the post-Golgi traffic and how the different GPCRs get sorted — in this case α2A and α2B, both adrenergic receptors involved in blood pressure regulation — and is watching the intracellular action in real time.
“Every time you look at these two receptors, you see this protein sitting with them,” Wu says of the clearly important C1orf27. In fact, the reason he’s also focusing on ufmylation is because of its also clear relationship with C1orf27, which he thinks regulates ufmylation. He is looking further at the interactions between the nascent protein and C1orf27 as well as ufmylation, which he has evidence are essential to the future GPCR’s ability to get out of the endoplasmic reticulum, to travel and mature.
As an example, when they used the gene editing technique CRISPR to remove C1orf27, the expression of adrenergic receptors was significantly reduced on the surface of embryonic kidney cells, while other receptor type numbers were unaffected. When they added them back, the usual adrenergic receptor population was restored, Wu says.
Further downstream, he thinks the protein HCR1 specifically regulates the α2A receptor then moving from the Golgi to the cell surface, that GGA3 helps α2B make the trip and that their pairing with these different proteins helps enable formation of the two distinct but similar receptors. Wu is working now to learn more about how the HCR1 binds to α2A, see if that initial bond is permanent and what happens to the receptor when HCR1 is MIA. Once he finds the binding method, his lab also will make moves like swapping it for the binding method used between GGA3 and α2B to see if maybe there is some kind of interaction between HCR1 and GGA3 that enables the important mobility of these developing receptors as they get closer to their destination. In fact, he wants to know whether the two together actually enable the delivery of the two sister receptors out of the Golgi and onto the surface, or if the two receptors take different paths — and taxis — to the surface only to end up side-by-side. So he is watching the taxis the developing receptors get on, and whether or not sometimes they ride together.
“Our research is very, very basic science,” adds Wu, who is among of small number of scientists focusing on the strategic moves of developing GPCRs. “Of course the long-term goal is to generate something good for disease treatment.”
GPCRs may not only contribute to disease by never reaching the cell surface, but also by making an early exit from the surface. In heart failure, for example, a condition that can result from coronary artery disease and heart attack where the heart can no longer pump sufficient blood and oxygen to the body, the beta adrenergic receptor on heart cells get hyper-activated to the point that the receptors move inside the cell to escape, Wu says. If this happens to enough cells, the heart can’t function.
The receptor’s movement back inside the cell for recycling or to be degraded because of reasons like overstimulation or just because its lifecycle is over, is a major point of research on these receptor types.
###
Media Contact
Toni Baker
[email protected]




