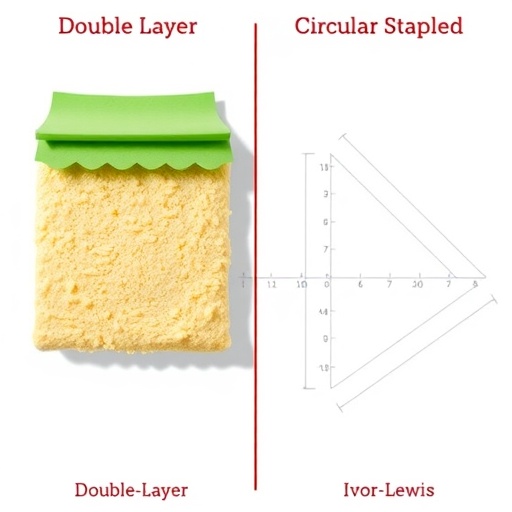
In a groundbreaking retrospective cohort study published in BMC Cancer, researchers unveil a promising surgical innovation for treating cancers of the lower esophagus and esophagogastric junction (EGJ)—areas notorious for their aggressive behavior and poor patient prognoses. The study compares the clinical outcomes of a novel double-layered scallop-shaped anastomosis (DLSSA) technique against the conventional circular stapled esophagogastric anastomosis (CSEA) in minimally invasive Ivor–Lewis surgery, shedding new light on strategies to mitigate one of the most feared post-surgical complications: anastomotic leakage (AL).
Esophageal and EGJ cancers maintain some of the most dismal survival rates in oncology, with surgery remaining the cornerstone of curative treatment. The minimally invasive Ivor–Lewis esophagectomy (MIIL) has emerged as a preferred approach due to its reduced morbidity. However, despite advancements, the challenge of anastomotic leakage—a breach in the surgical connection between the esophagus and stomach—continues to jeopardize patient outcomes, increasing morbidity and mortality despite surgical progress.
Addressing this critical issue, the study conducted a detailed retrospective analysis between April 2016 and February 2023 involving 117 patients who underwent MIIL. These subjects were divided into two cohorts: 50 patients received the innovative DLSSA approach, while 67 patients underwent the standard CSEA technique. The study meticulously compared intraoperative parameters, postoperative complications, and specifically the incidence of anastomotic leakage between the two groups, aiming to establish whether DLSSA offers a tangible clinical advantage.
.adsslot_ryH5leXf8E{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_ryH5leXf8E{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_ryH5leXf8E{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Technically, the DLSSA technique features a double-layered anastomosis with a scallop-shaped configuration, a departure from the traditional, circular stapling method that mechanically joins the esophagus to the stomach. The double-layer approach theoretically provides enhanced mechanical integrity and promotes superior tissue apposition, potentially reducing micro-leaks and enhancing vascularization at the anastomotic site.
Surgical duration was comparable between the two groups, averaging approximately 280 minutes, indicating that adoption of the DLSSA technique does not impose additional operative time. However, intraoperative blood loss was statistically lower in the DLSSA cohort (100 ml) compared to the CSEA group (120 ml), a difference with clinical importance suggesting less intraoperative trauma or enhanced hemostasis.
Postoperative complications occurred at a similar frequency overall—32.5% across all patients—reflecting the complexity and inherent risks associated with esophageal surgery regardless of the anastomotic technique. Crucially, however, the incidence of anastomotic leakage was significantly reduced in the DLSSA group, with only 4.0% experiencing AL versus a notable 17.9% in the CSEA cohort. This striking reduction underscores the potential of the DLSSA configuration to confer superior anastomotic security.
Interestingly, while the DLSSA group exhibited a lower rate of AL, it also demonstrated a higher incidence of pleural effusion (10.0% vs. 1.5% in CSEA). This relationship warrants further investigation to understand the physiological or technical factors that may predispose patients to fluid accumulation postoperatively, balancing the benefits of reduced leakage against this emerging complication.
To elucidate predictors of anastomotic leakage risk, multivariable binary logistic regression analysis was performed, revealing that higher body mass index (BMI) significantly increased the risk of AL, consistent with existing literature citing obesity as a surgical risk factor. Conversely, undergoing DLSSA was independently associated with markedly reduced odds of AL, verifying that the novel technique itself imparts a protective effect beyond patient-related risk factors.
The authors emphasize that the novel DLSSA technique’s scaffolding effect likely reinforces the anastomotic junction, diminishes tension points, and optimizes blood supply continuity—factors critical in wound healing and prevention of leak formation. By creating a scalloped, double-layered configuration, DLSSA effectively redistributes mechanical stresses and may reduce ischemic vulnerabilities inherent in traditional circular stapling.
Given these promising outcomes, the study heralds the DLSSA technique as a potentially safer alternative in thoracoscopic Ivor–Lewis surgery, potentially setting a new standard in esophagogastric anastomosis. However, the retrospective nature of the analysis calls for prospective randomized clinical trials to validate these findings, assess long-term survival and functional outcomes, and refine procedural protocols.
Further research is also necessary to optimize perioperative management addressing the elevated pleural effusion risk identified, potentially through refined intraoperative techniques, enhanced drainage strategies, or adjunct medical therapies. Understanding the pathophysiology underlying this complication will be crucial for holistic improvement in postoperative recovery and patient quality of life.
This study’s implications extend beyond esophageal surgery, as anastomotic integrity remains a crucial determinant of outcomes across gastrointestinal surgical procedures. The concept of double-layered, shape-modified anastomoses may inspire innovations in surgical techniques for other challenging anatomic sites where leakage risk is unacceptably high.
Ultimately, the authors advocate an integrated surgical paradigm combining meticulous technique with patient-specific risk stratification—such as BMI assessment—to tailor interventions, mitigate leakage risk, and improve prognosis for patients afflicted by these devastating cancers. With minimally invasive approaches gaining traction, refined anastomotic methods like DLSSA may catalyze a paradigm shift in complex esophageal cancer surgeries.
As oncologic surgery evolves, the balance between technical innovation and rigorous clinical validation will be imperative. The pioneering work by Li et al. thus represents a milestone in this journey, offering hope to patients and clinicians striving to conquer the formidable challenges posed by esophageal and EGJ malignancies in the modern surgical era.
Subject of Research: Comparison of double-layered scallop-shaped anastomosis (DLSSA) and circular stapled esophagogastric anastomosis (CSEA) techniques in minimally invasive Ivor–Lewis surgery for distal esophageal and esophagogastric junction cancers.
Article Title: Comparison of double-layered scallop-shaped anastomosis and circular stapled anastomosis in Ivor–Lewis surgery for esophageal and EGJ cancer: a retrospective cohort study
Article References:
Li, K., Yang, Q., Wang, Y. et al. Comparison of double-layered scallop-shaped anastomosis and circular stapled anastomosis in Ivor–Lewis surgery for esophageal and EGJ cancer: a retrospective cohort study. BMC Cancer 25, 1035 (2025). https://doi.org/10.1186/s12885-025-14437-w
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14437-w
Tags: advancements in cancer surgery techniquesanastomotic leakage prevention strategiescircular stapled esophagogastric anastomosisdouble-layer scallop-shaped anastomosisesophageal cancer surgical outcomesesophagogastric junction cancer treatmentinnovative surgical techniques for cancerminimally invasive Ivor-Lewis surgerymorbidity and mortality in esophageal surgeriespatient prognosis in esophageal surgeryretrospective cohort study in oncologysurgical complications in MIIL