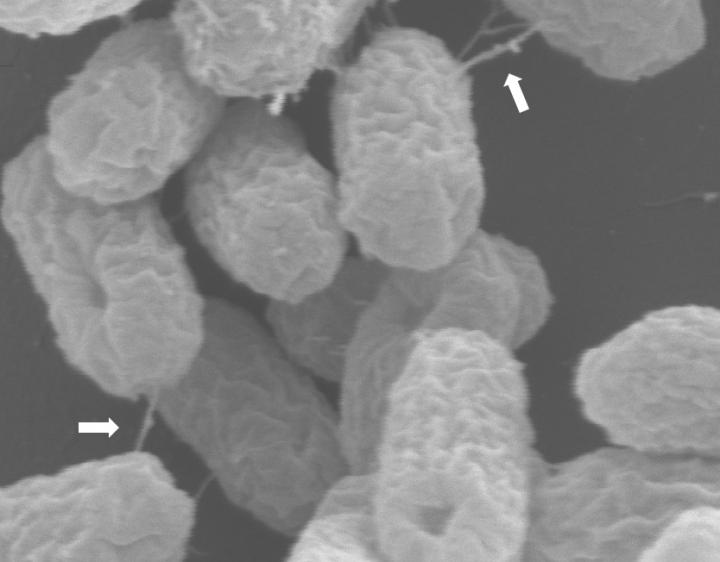
Credit: Professor Mark Schembri
There is new hope for approximately 700,000 people who die each year from antibiotic resistant infections, with University of Queensland researchers discovering how bacteria share antibiotic-resistance genes.
UQ’s Professor Mark Schembri said antibiotic resistant bacteria, in particular emerging ‘superbugs’, could lead to around 10 million deaths globally by 2050.
“The diminishing pool of effective antibiotics makes these infections a major threat to human health, so it’s critical we understand the exact mechanics of how antibiotic resistance spreads between different bacteria,” Professor Schembri said.
“In this study, we examined plasmids – self-replicating DNA molecules – which are one of the major drivers for the rapid spread of antibiotic resistance genes between bacteria.
“Many plasmids carry 10 to 15 antibiotic resistance-causing genes, and when they transfer from one bacterial cell to another, two important things happen.
“Firstly, the plasmid is copied so that it is retained by both the donor and recipient cell, and secondly all antibiotic resistance genes are transferred together, meaning that resistance to multiple antibiotics can be transferred and acquired simultaneously.”
Lead author Dr Steven Hancock said the study used a powerful genetic screening system to identify all of the components required for the transfer of an important type of antibiotic resistance plasmid from one bacterial cell to another.
“Our investigation discovered genes encoding the ‘syringe’ component,” Dr Hancock said.
“That is the mechanism through which plasmid DNA is mobilised, as well as a novel controlling element essential for regulation of the transfer process.”
The team also investigated the crystal structure of this controlling element, and revealed how it binds to DNA and activates transcription of other genes involved in the transfer.
Professor Schembri said this deeper understanding would open the door to solutions for this ever-growing health crisis.
“Preventing the transfer of plasmids between bacteria has been a major challenge in reducing the spread of antibiotic resistance genes,” he said.
“By looking at the molecular mechanics, we can start to develop effective solutions for stopping these genes in their tracks.
“Almost everyone has suffered an infection that did not respond to a first round of antibiotic treatment, only to be fortunate enough to be treated with a different antibiotic that worked.
“Now, in extreme cases, we’re seeing common infections caused by superbugs that are resistant to all available antibiotics, highlighting the increasing challenge of antibiotic resistance.
“We need to tackle this now, and I’m excited to see how this new knowledge will lead to novel approaches, potentially saving millions of lives globally.”
###
The research has been published in Nature Microbiology (DOI: 10.1038/s41564-020-0775-0).
The multidisciplinary team included researchers from the UQ School of Chemistry and Molecular Biosciences, the UQ Centre for Clinical Research, the UQ Institute for Molecular Bioscience, the University of Melbourne and the University of Oxford.
Media Contact
Professor Mark Schembri
[email protected]
Related Journal Article
http://dx.




