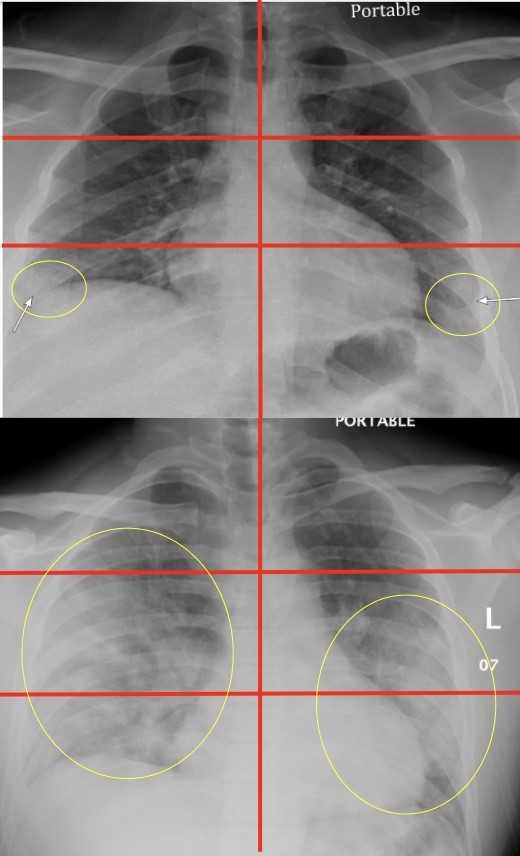
Top image: Chest radiograph of a 23-year-old male with no past medical history who tested positive for COVID-19 via RT-PCR and was subsequently discharged from the emergency department with home…
view more
Chest X-rays performed on young and middle-aged adults with COVID-19 when they arrive at the emergency room can help doctors predict who is at higher risk of severe illness and intubation, Mount Sinai researchers report.
The first-of-its kind study, published in the May 14 issue of Radiology, identifies which patients may need to be hospitalized and intubated based on the severity of coronavirus patterns in the lungs seen in the X-rays, using a unique scoring system to evaluate severity. The results could help physicians more quickly identify, triage, and aggressively treat these high-risk patients.
“This is the first study looking at how we can use chest X-rays from the emergency room to predict how sick COVID-19 patients will get. We demonstrate how valuable X-rays can be during this pandemic because, by evaluating disease in different portions of the lungs, we can predict outcomes, which can potentially help appropriately allocate resources and expedite treatment in the most severe cases,” says first author Danielle Toussie, MD, resident in the Department of Radiology at the Icahn School of Medicine at Mount Sinai.
“We came up with the scoring system because we had clinicians asking us what we see on chest X-rays of COVID-19 patients,” Dr. Toussie says. “We would tell them, ‘We see this opacity here or that opacity there,’ but then they would ask, ‘What does that mean for my patient?’ That’s what we set to find out, and we started noticing that while most patients had disease in the lower lobes only, the patients who had multiple areas of disease, or disease in the upper lobes, seemed to be doing worse. So we devised a way to divide the lungs up, score them for severity of disease, and correlate that with what actually happened to the patients as the disease progressed or resolved.”
A team of radiologists analyzed records of 338 COVID-19-positive patients at The Mount Sinai Hospital, Mount Sinai Queens, and Mount Sinai Brooklyn between March 10 and March 26. Patients were between the ages of 21 and 50 (average age 39) and 62 percent male. Researchers had access to information including race and pre-existing conditions such as asthma, diabetes, hypertension, HIV, and obesity. All patients had an X-ray taken in the emergency room.
Investigators focused on every patient’s chest X-ray to examine patterns of coronavirus in their lungs, looking at the opacities (white circular markings associated with COVID) and where those patterns lay. Researchers divided the X-rays into six zones (upper right, upper left, middle right, middle left, lower right, and lower left) and developed a scoring system from zero to six to quantify severity. The total score depended on how many zones disease showed up in. Lower severity scores ranged from zero to two, and higher severity from three to six.
Of the 338 patients, 145 were admitted. Patients with highest chest X-ray scores were 6.2 times more likely to require hospitalization, and 4.7 times more likely to be intubated. A more specific breakdown showed that of the 34 patients with a “zero” score, two were intubated; out of the 15 patients with a “one” score, one was intubated; 38 patients had a score of “two,” and six were intubated; of the 14 patients with a score of “three,” two were intubated; out of 32 patients with a score of “four,” 10 were intubated; for the seven patients with a score of “five,” three were intubated, and four of the five patients with a score of “six” were intubated.
Men were more likely than women to have higher chest X-ray scores and be admitted, but were not more likely to be intubated. Obese patients were also more likely to have higher chest X-ray scores and require hospitalization.
The analysis went on to show that patients at Mount Sinai Queens were more likely to have more severe disease and require intubation compared to patients in Manhattan or Brooklyn. Despite prior reports describing worse outcomes in African Americans and Latinos, this study showed no significant differences in outcomes between patients of different race and ethnicity when adjusted for other factors such as age, gender, comorbid medical conditions, and weight.
“This study provides particular insight on how some of the younger demographic, who still make up a sizable proportion of those affected by the virus, may fare upon presentation to the emergency room, allowing for efficient mobilization of available means of treatment,” says co-author Yogesh Sean Gupta, MD, Associate Professor of Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine at Mount Sinai.
“These findings underscore how COVID-19, despite its many manifestations, is largely a respiratory illness and the lung changes identifiable on X-ray are a primary predictor of disease progression,” adds senior author Adam Bernheim, MD, Assistant Professor of Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine at Mount Sinai. “This work is foundational for demonstrating the role of radiology not only in diagnosis, but also in predicting, triaging, and risk-stratifying COVID-19 patients so that those at highest risk for severe disease can be immediately identified from the moment of the very first chest X-ray upon presentation.”
Cardiothoracic radiologists at Mount Sinai have implemented this scoring system in clinical practice, helping emergency physicians classify patients accordingly.
###
The BioMedical Engineering and Imaging Institute at Mount Sinai also contributed to this research.
About the Mount Sinai Health System
The Mount Sinai Health System is New York City’s largest academic medical system, encompassing eight hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. Mount Sinai is a national and international source of unrivaled education, translational research and discovery, and collaborative clinical leadership ensuring that we deliver the highest quality care–from prevention to treatment of the most serious and complex human diseases. The Health System includes more than 7,200 physicians and features a robust and continually expanding network of multispecialty services, including more than 400 ambulatory practice locations throughout the five boroughs of New York City, Westchester, and Long Island. The Mount Sinai Hospital is ranked No. 14 on U.S. News & World Report’s “Honor Roll” of the Top 20 Best Hospitals in the country and the Icahn School of Medicine as one of the Top 20 Best Medical Schools in country. Mount Sinai Health System hospitals are consistently ranked regionally by specialty by U.S. News & World Report.
For more information, visit https:/
Media Contact
Ilana Nikravesh
[email protected]




